Propranolol
Waldo C. Feng, MD, PhD, FACS, FAAP
- Clinical Professor, University of Nevada Medical School
- Chief of Urology, Sunrise Hospital and Children’s Medical
- Center, Las Vegas, Nevada
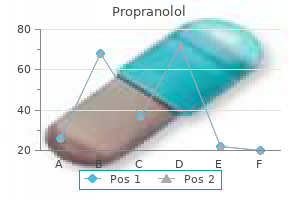
Propranolol dosages: 80 mg, 40 mg, 20 mg
Propranolol packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

20mg propranolol visa
Efficacy of coupled low-volume plasma trade with plasma filtration adsorption in treating pigs with acute liver failure: a randomised examine capillaries leaking cheap 40 mg propranolol with amex. Outcomes and complications of intracranial pressure monitoring in acute liver failure: a retrospective cohort study capillaries ks2 buy 20 mg propranolol with mastercard. The impact of hypertonic sodium chloride on intracranial strain in sufferers with acute liver failure arteries synonym cheap propranolol 20mg without prescription. Moderate hypothermia in patients with acute liver failure and uncontrolled intracranial hypertension. Fulminant hepatic failure secondary to acetaminophen poisoning: a scientific evaluate and meta-analysis of prognostic criteria figuring out the necessity for liver transplantation. Acute liver failure: scientific features, consequence evaluation, and applicability of prognostic criteria. Optimization of mass switch for toxin removing and immunoprotection of hepatocytes in a bioartificial liver. Controlled trials of charcoal hemoperfusion and prognostic factors in fulminant hepatic failure. Artificial liver support system utilizing large buffer volumes removes important glutamine and is an ideal bridge to liver transplantation. Albumin dialysis in cirrhosis with superimposed acute liver damage: a prospective, managed research. Pathophysiological effects of albumin dialysis in acute-on-chronic liver failure: a randomized controlled research. Albumin dialysis with a noncell artificial liver support system in sufferers with acute liver failure: a randomized, controlled trial. Tzakis 129 resuscitation is required for sufferers presenting with intraperitoneal or gastrointestinal hemorrhage. Aneurysms of the extrahepatic portion of the artery are classically managed surgically. Despite advancements in endovascular technology, open restore stays the mainstay of therapy. Those originating distal to the gastroduodenal artery, affecting the proper hepatic artery, may be treated by aneurysmectomy and revascularization of the liver. A pseudoaneurysm of the hepatic artery following liver transplantation on the web site of the arterial anastomosis is a critical complication. The traditional treatment is resection of the pseudoaneurysm and revascularization of the liver. This method is especially useful if the lesions are multiple, as seen in circumstances of polyarteritis nodosa. They could be arbitrarily categorised into people who involve the hepatic artery and its branches, people who involve the portal vein, and those that involve the hepatic veins. The subjects portal hypertension and portal vein thrombosis are addressed individually in Chapter a hundred thirty five. True aneurysms could also be a manifestation of systemic ailments, together with atherosclerosis or vasculitides such as polyarteritis nodosa1 and systemic lupus erythematosus. Most generally, hepatic artery aneurysms are solitary, contain the extrahepatic portion of the artery, and are three to 4 cm in diameter on the time of presentation. Patients with mycotic pseudoaneurysms could present with ache, fever, or other signs of an infection. Hemobilia following laparoscopic cholecystectomy,four liver biopsy, or interventional radiologic procedures may result from rupture of a pseudoaneurysm into the biliary tree. Intraperitoneal or gastrointestinal hemorrhage�related rupture is related to a high mortality price. Angiography could be diagnostic, and with the help of endovascular strategies, could be therapeutic as nicely. Although the natural history of these aneurysms is unclear, plainly dimension correlates with the chance of rupture. In addition, the ever present use of high-quality imaging methods has led to an increased detection of small, asymptomatic aneurysms. The concern of eventual problems, particularly hemorrhage, warrants the consideration of treating all of those lesions, even those that are asymptomatic or are found by the way. Penetrating accidents to the portal triad outnumber blunt accidents, and associated injuries are the rule. Portal triad injuries carry a high mortality rate because of exsanguinating hemorrhage or refractory shock. Successful remedy requires management of bleeding, aggressive resuscitation, and temporization of other injuries. Better survival has been reported with hepatic artery ligation as compared with repair. The subjects portal hypertension and portal vein thrombosis are addressed separately in this quantity. Hepatic artery problems embody aneurysms of the hepatic artery, arterial injury from penetrating trauma or iatrogenic procedure-related trauma, hepatic artery thrombosis within the context of liver transplantation, and arterioportal and arteriovenous shunts. Other than portal hypertension and portal vein thrombosis, portal vein problems are uncommon, however embrace aneurysms of the portal vein. The addition of an harm to the artery was thought to portend the next complication rate after biliary reconstruction and a higher danger of mortality. In the affected person presenting with bile duct strictures after cholecystectomy, the presence of a concomitant arterial injury ought to be suspected based on the severity of the bile duct injury and the discovery of a report of problem gaining hemostasis during the cholecystectomy. The treatment of those accidents is normally directed towards repairing the bile duct endoscopically by primary restore or by Roux-en-Y hepaticojejunostomy. Arterial reconstruction, besides when the injury is noted immediately, is seldom indicated or performed. Rarely, an damage to the best hepatic artery results in acute necrosis of the right hepatic lobe or intrahepatic strictures amenable to hepatic resection. With an incidence of 2% to 8% of cases, it has a high associated morbidity and mortality. Pediatric recipients23 and circumstances requiring aortohepatic conduits24 are at increased danger for the development of this complication. Advanced donor age increases the danger of liver graft loss from hepatic artery thrombosis. For others, the sequelae are biliary tract problems, together with stricture formation, bile leak, cholangitis, hemobilia, and hepatic biloma/ abscess. Cholangitis may be managed by percutaneous or endoscopic catheter decompression of the biliary tree. Attempts at biliary reconstruction or hepatic artery revascularization are rarely profitable. Although some asymptomatic patients spontaneously develop arterial collaterals and can be handled conservatively, most survivors with late hepatic artery thrombosis will ultimately require retransplantation. When detected, it may be addressed with endovascular techniques, together with percutaneous transluminal angioplasty or main stent placement, avoiding the dire issues of thrombosis. These shunts may result from iatrogenic injury,29 penetrating or blunt liver trauma,30 benign and malignant hepatic neoplasms, or might develop congenitally,31 such as in sufferers with hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber disease).
Diseases
- Macular dystrophy, vitelliform
- Alopecia immunodeficiency
- Meretoja syndrome
- Chromosome 6, trisomy 6q
- Ahumada-Del Castillo syndrome
- Plum syndrome
- Richieri Costa Orquizas syndrome
Generic propranolol 20mg with amex
After being extracted by the hepatocytes cardiovascular key terms purchase propranolol 80 mg without prescription, bilirubin is conjugated with glucuronic acid to form bilirubin diglucuronide (conjugated bilirubin) cardiovascular system gcse edexcel discount 40 mg propranolol overnight delivery. The enzyme liable for this reaction is glucoronil transferase current in the endoplasmic reticulum of the hepatocyte cardiovascular week purchase 40 mg propranolol fast delivery. Bilirubin is then transported inside the hepatocyte by cytosolic binding proteins, delivering the molecule to the canalicular membrane for active secretion into bile. Conjugated bilirubin is then excreted into the duodenum in association with combined lipid micelles. Once within the intestine, bilirubin is transformed to urobilinogens by intestinal bacteria, which are then further oxidized to pigmented urobilins. To serve this general operate, the gallbladder has absorptive, secretory, and motor capabilities. As a outcome the gallbladder stores concentrated bile that reenters the distal bile duct and is secreted into the duodenum in response to a meal. The resultant mucin gel is believed to represent an necessary part of the unstirred layer (diffusion-resistant barrier) that separates the gallbladder cell membrane from the luminal bile. However, considerable proof additionally suggests that mucin glycoproteins play a job as pronucleating brokers for cholesterol crystallization. Bile is usually concentrated fivefold by the absorption of water and electrolytes. The concentration of calcium in gallbladder bile, which is a vital factor in gallstone pathogenesis, is influenced by serum calcium, hepatic bile calcium, gallbladder water absorption, and the focus of organic substances, such as bile salts in gallbladder bile. The solubility in the micellar fraction is elevated, but the stability of phospholipid-cholesterol vesicles is significantly decreased. Because ldl cholesterol crystal precipitation occurs preferentially by vesicular rather than micellar mechanisms, the web effect of concentrating bile is an increased tendency to nucleate ldl cholesterol. However, the absorption of bilirubin, cholesterol, phospholipids, and bile salts is minimal compared with that of water. Thus these organic compounds are significantly concentrated by the conventional absorptive course of that happens within the gallbladder. The arrows point out the route of water move across the cell membrane and into the intercellular spaces. As water is transported into the house, the space distends, and an isotonic solution enters the connective tissue house. Prostaglandins play an essential role as stimulants of gallbladder mucin secretion. Furthermore, mucin glycoproteins are key pronucleating agents for ldl cholesterol crystallization. The acidification of bile happens by the transport of hydrogen ions by the gallbladder epithelium, via a sodium-exchange mechanism. Acidification of bile promotes calcium solubility, thereby preventing its precipitation as calcium salts. Compared with gallbladder bile, the bile secreted by the liver is slightly alkaline, pH 7. When stimulated by consuming, the gallbladder empties 50% to 70% of its contents within 30 to forty minutes. Many other hormonal and neural pathways are also needed for the coordinated motion of the gallbladder and sphincter of Oddi. Defects in gallbladder motility, which increase the residence time of bile in the gallbladder, play a central function in the pathogenesis of gallstones. Endoscopic sphincterotomy: follow-up evaluation of results on the sphincter of Oddi. The sphincter regulates the flow of bile and pancreatic juice into the duodenum and likewise prevents the regurgitation of duodenal contents into the biliary tract. These features are achieved by maintaining strain throughout the bile and pancreatic ducts greater than duodenal strain. Thus sphincter pressure relaxes after a meal, allowing the passive flow of bile into the duodenum. During fasting, high-pressure phasic contractions of the sphincter of Oddi persist through all phases of the migrating myoelectric complex. Variations in origin and course of the hepatic artery and its branches: importance from a surgical viewpoint. Intestinal diffusion barrier: unstirred water layer or membrane surface mucous coat Recent progress in understanding ldl cholesterol crystal nucleation as a precursor to human gallstone formation. Interdigestive biliary output in man: relationship to fluctuations in plasma motilin and impact of atropine. This activity may be a preventive mechanism towards the accumulation of biliary crystals during fasting. The cholecysto�sphincter of Oddi reflex allows the human sphincter to loosen up as the gallbladder contracts. The gross anatomy and histology of the gallbladder, extrahepatic bile ducts, vaterian system, and minor papilla. The hepatic, cystic, and retroduodenal arteries and their relations to the biliary ducts with samples of the entire celiacal blood supply. The cystic artery and constituents of the hepatic pedicle: a examine of 500 specimens. Practical classification of the branching forms of the biliary tree: an evaluation of 1094 consecutive direct cholangiograms. A thorough analysis of a affected person with obstructive jaundice consists of detailed medical and surgical historical past, bodily examination, laboratory data, and analysis of pertinent imaging. A multidisciplinary method including the primary care physician, surgeon, gastroenterologist, and interventional radiologist offers complete administration options. Noninvasive imaging studies provide the inspiration for remedy planning, together with surgical and/or percutaneous intervention. Percutaneous biliary interventions will be the primary diagnostic and therapeutic therapy option or serve as a conduit for later surgical intervention. The principal goals of the chapter include (1) reviewing the position of noninvasive imaging modalities commonly used in the affected person presenting with biliary obstruction and (2) inspecting the position of minimally invasive percutaneous interventions obtainable for the patient with either benign or malignant biliary disease. The goals of imaging are to not only affirm the presence of obstructive jaundice but additionally to define the biliary anatomy. In the case of a malignant etiology, imaging can even stage the extent of illness. These methods, as nicely as different interventions, together with percutaneous biopsy, drainage catheter management, percutaneous biliary stricture dilatation, and biliary endoprostheses, are reviewed. The aim of the chapter is to provide readers with a fundamental understanding of the position of imaging and imageguided intervention for the affected person with advanced biliary situations. The regular gallbladder is an ovoid, anechoic, fluid-filled construction adjoining to the interlobar fissure, which separates the best and left hepatic lobes. The cystic duct is generally positioned posterior to and may be a part of with the widespread hepatic duct at variable distances, forming the common bile duct. The hepatic artery separates the frequent hepatic duct from the portal vein inside the hepatoduodenal ligament.
Propranolol 40 mg low cost
Sudden publicity of the center to cold heart disease x ray buy propranolol 40 mg otc, hyperkalemic fluid and the milieu of cytokines released from the transplanted organ are the doubtless causes cardiovascular disease tests purchase propranolol 20 mg overnight delivery. An ominous sign is that of an escalating pulmonary artery stress related to a falling systolic blood stress heart disease essay purchase propranolol 80mg without a prescription. This scenario is extra frequent in recipients with preexisting pulmonary hypertension, diastolic dysfunction, or another condition leading to mounted cardiac output or restricted cardiac reserve. Although the best measure is to forestall extreme reperfusion syndrome, it might be unavoidable in certain circumstances, especially when combining marginal organs with sick recipients. The vascular anastomoses are inspected individually, along with the retroperitoneal space along the diaphragmatic attachments and the bare space. A dramatic improvement can be effected with launch of the celiac axis from this ligament at its origin off the aorta. Graft Function and Primary Nonfunction the assessment of graft operate depends on medical indicators, laboratory analysis, and a certain quantity of intuition. In the perfect situation, the graft shows a healthy perfusion pattern and starts producing bile inside half-hour of reperfusion. Over the next 12 to 24 hours, acidosis ought to resolve, and hemodynamics, mental status, and urine output ought to improve. When a transplanted organ reveals indicators of dysfunction in the first several hours or days after transplant, several components should be thought-about. Although most grafts do present no less than partial function, the indicators and signs of a truly nonfunctional graft are easy to acknowledge. These grafts seem hyperemic, "blebbed," and firm, and will fracture with manipulation. Recipient acidosis, persistent vasodilation, renal failure, coagulopathy, and even cerebral edema might happen. In excessive circumstances, if no appropriate alternative organ is out there and a patient is unstable, removal of the nonfunctional graft and creation of a temporary portacaval shunt may enable the patient to stabilize. This anhepatic state represents a true emergency, and survival without a new liver is often lower than forty eight hours. Other manipulations, corresponding to plasmapheresis or utilization of experimental synthetic hepatic support units have been tried with various levels of success. In different instances, graft dysfunction leads to a cascade of events resulting in multiorgan dysfunction syndrome and a "failure to thrive," which may in the end result in sepsis and death. It is up to the transplant team to weigh the risks of watchful waiting versus that of retransplantation. Definitive analysis is commonly obtained by surgical exploration, angiography, or cross-sectional imaging. Strictures at this stage can often be managed with endoscopic or percutaneous interventional radiology methods, however sometimes surgical revision with hepaticojejunostomy is required. Intrahepatic strictures and those which are distant from the anastomosis typically reflect a extra diffusely diseased biliary tree. Many grafts with intrahepatic strictures can be temporized with aggressive and repeated percutaneous or endoscopic interventions, however some would require repeat transplantation because of recurrent cholangitis or secondary biliary cirrhosis. If the bile leak is of a large quantity or is associated with peritonitis, surgical repair ought to be tried promptly. A expert endoscopist or radiologist can typically handle smaller volume leaks by stenting the anastomosis and decompressing the biliary tree. The augmented immunosuppression used to treat rejection is believed to play a role in viral replication and the more aggressive return of viral hepatitis. Chronic rejection is a poorly understood entity often referred to as "vanishing bile duct syndrome. Not surprisingly, the use of medications designed to disrupt immune competence puts individuals at elevated danger for an infection. The nature of that risk depends on numerous parameters including the interval since transplantation, the intensity of immunosuppression, preexisting exposures to certain infectious agents, the age of the recipient, and the character and extent of other comorbid conditions (Table 127. As with different surgical procedures, the chance for bacterial infections is best in the first few weeks after transplant. Because of their impaired cell-mediated immunity, transplant sufferers stay at greater than normal risk for viral and fungal infections for life. Prophylactic antibiotics are given after transplant, although the exact agent and duration varies among programs. This agent was once a standard reason for morbidity and demise of liver transplant however is now seen with an incidence of lower than 5%. Although the precise mechanisms are nonetheless incompletely understood, immunosuppression clearly increases the risk of some types of malignancy. Treatment options embrace merely rising the upkeep immunosuppression in delicate instances, and initiating a steroid pulse in cases which are more extreme. All transplant sufferers ought to bear vigilant screening for breast, prostate, colorectal, gynecologic, and skin cancer. Cardiovascular Side Effects Cardiovascular illness has become one of many leading causes of long-term morbidity in liver transplant survivors. Only after the shortage of organs reached a important threshold was consideration given to performing such a process, which poses substantial perioperative and maybe long-term risks to the healthy donor. Many moral points continue to be raised including the age, relationship to recipient, and the social circumstances of potential donors. First, transplantation may be timed to intervene before a recipient becomes severely decompensated, thereby minimizing the risks of certain issues, avoiding repeated hospitalizations, and even minimizing costs. Second, the quality of the allograft should be optimum with minimal cold ischemia and with out the physiologic insults usually suffered by deceased donors. On the opposite hand, the comparatively smaller quantity and the elevated technical anastomotic challenges offered by partial grafts create a model new set of potential recipient issues. Add to that probably the most paramount concern of donor well being, and some nice advantages of living versus deceased donors turn out to be less distinct. The most compelling objection focuses on the morbidity and mortality danger related to live liver donation. In a survey of seventy one transplant applications that carried out 11,553 donor hepatectomies, Cheah et al. A description of the living donor partial hepatectomy and the dwelling donor transplant procedure is beyond the scope of this chapter. There are ongoing efforts to improve the deceased donor organ pool by a quantity of different distinct pathways. The first approach is to improve the variety of potential donors by improving intensive care unit and resuscitation protocols for sufferers with lethal mind damage, in order that organ quality is maintained till organ recovery can be coordinated. The second method is to decrease the variety of donors that are lost due to lack of household consent through the use of a selection of public academic and public well being measures. These marginal, or "prolonged criteria" donors, include older or much less hemodynamically stable donors, non-heartbeating donors, or these with comorbid situations such as extreme hepatic steatosis.
Purchase 80 mg propranolol with amex
When rupture occurs cardiovascular key terms cheap propranolol 40 mg with amex, the affected person might current with sudden cardiovascular collapse and shock cardiovascular disease signs and symptoms buy propranolol 80 mg low price, normally preceded by acute pain; nonetheless cardiovascular disease statistics 2015 purchase propranolol 40mg with visa, a "double rupture phenomenon" can occur. Later, when free intraperitoneal extravasation of blood happens with loss of tamponade, the affected person progresses to profound hemorrhagic shock and possible demise. Increased collagen lysis after laparotomy has been associated with visceral aneurysm rupture in the first week after liver transplantation. If found, the recommendation is to deal with these patients during the interval of liver transplantation. Physical examination findings may embody tenderness over the uterine fundus, making the analysis more difficult. Diagnosis A plain radiograph may reveal the calcified splenic artery aneurysm by displaying the basic signet ring�shaped calcifications within the left upper quadrant. It is the preferred modality in being pregnant due to decreased danger to the fetus from ionizing radiation and can be utilized in any symptomatic patient to detect free fluid within the left upper quadrant. Catheter angiography with number of the visceral vessels is a useful diagnostic and doubtlessly therapeutic tool within the armamentarium of the interventionalist or vascular surgeon. However, using intravascular distinction media is contraindicated in being pregnant because of the danger to the developing fetus. In common, all asymptomatic splenic artery aneurysms ought to be handled when greater than 2 cm in diameter. The timing of intervention for an asymptomatic splenic artery aneurysm found throughout pregnancy is a difficult choice, however surgery in the course of the second trimester is assumed to be associated with the least risk to the creating fetus. The selection of therapy could depend upon such components as anatomic location, acuity of signs, clinical presentation, and patient and doctor desire. Large single-center sequence reveal the increasing choice to treat these lesions with endovascular strategies. Indeed, a big systematic review of more than 1300 splenic aneurysms treated with both open surgical, endovascular, or conservative therapy revealed endovascular strategies to have a much lower incidence of short-term problems and a considerably shorter hospital keep in contrast with open methods. Challenges for endovascular stent grafting are a wide neck of the aneurysm and splenic artery tortuosity. Complications include stent graft thrombosis, infection, and access-related issues. If the hilum is involved, embolization is generally not profitable, and splenectomy could additionally be beneficial. It can occur in 30% of patients and presents as fever, extreme belly pain, ileus, and, often, pancreatitis. Simple ligation of the proximal splenic artery is inadequate for remedy of an aneurysm within the splenic hilum because collateral flow through accessory splenic or gastroepiploic arteries will continue to perfuse the aneurysm. The laparoscopic strategy is contraindicated if the patient is hemodynamically unstable or with evidence of rupture. For distal aneurysms, a laparoscopic lateral strategy facilitates visualization of the aneurysm, use of the endoscopic stapler, and splenectomy. In addition, supraceliac control of the aorta can temporize bleeding until the splenic artery is managed. Delaying supply until the splenic artery bleeding is controlled is beneficial, but if cardiac arrest has occurred, prompt delivery of the fetus inside minutes is essential. However, pseudoaneurysms are more and more frequent, now accounting for almost half of all reported hepatic artery aneurysms. Anatomy and Pathology Historically, an infection was the commonest etiology for hepatic artery aneurysms, classically after intravenous drug abuse or intraabdominal infection. Some reports now estimate pseudoaneurysms to approach almost 50% of all hepatic artery aneurysms. Intrahepatic aneurysms in liver transplant sufferers are typically pseudoaneurysms at websites of biopsy or drainage. Of these patients who current with symptoms, right upper quadrant or epigastric pain is the most typical symptom, current in additional than 50%. Jaundice can even happen without rupture when the bile duct is extrinsically compressed by the aneurysm. Of these presenting with rupture, 50% may have rupture into the biliary tree and one-third current with the Quincke triad of stomach pain, hemobilia, and obstructive jaundice. If atherosclerotic changes have occurred, a hoop of calcifications could also be seen in the right upper quadrant on plain radiograph. Although the duodenum was adherent to the mass, there was no arterial-enteric fistula. Ultrasound may suggest a cystic construction that can be mistaken for a cystic tumor or pseudocyst; thus cautious shade circulate analysis is a vital software to distinguish a strong construction from a vascular construction. Angiography offers both information about the aneurysm and might consider for different intraabdominal aneurysms, that are present in 20% of patients. Patients with aneurysms and significant comorbidities have been followed, and none ruptured over a imply of 68. Extrahepatic aneurysms are sometimes treated surgically, whereas intrahepatic aneurysms are usually handled with endovascular techniques. Extrahepatic aneurysms can occasionally be handled with resection and grafting or aneurysmorrhaphy. Intrahepatic aneurysms might require liver resection if not amenable to endovascular methods. Similar to splenic artery aneurysms, endovascular catheter-based therapies are getting used extra incessantly but should face the problem of sustaining sufficient hepatic perfusion. Ligation or aneurysm resection with revascularization has been reported to be essential in 25% of elective procedures. Bowel resection is usually required for emergency circumstances when rupture or ischemia is current. Other reported causes are inflammatory processes within the abdomen or retroperitoneum (cholecystitis, pancreatitis) and trauma. In one report, practically 20% of sufferers had an identifiable collagen vascular dysfunction. They occur with equal frequency in men and women, and are usually identified within the fifth decade of life. Catheter angiography offers the power to determine the adequacy of collateral circulate and helps to set up both catheter-based or surgical options. Treatment Open surgical approaches to celiac artery aneurysms have included ligation alone, reimplantation, aneurysmorrhaphy, and grafting and is really helpful at diameters starting at 2 cm for asymptomatic lesions. Resection and reimplantation on the aorta or transposition to the iliac artery have also been reported. Initial selective catheterization of the widespread hepatic artery allowed for number of the gastroduodenal artery with a microcatheter and embolization with glue. There is additional glue present within the gastroepiploic artery, branches to the pancreas, and the gallbladder wall. When related to pancreatitis, most arise in males, normally within the fifth decade of life. Open methods include ligation, excision of the aneurysm with main reanastomosis, and aneurysmorrhaphy. Sometimes large mesenteric hematomas are current and might make finding the aneurysm a problem at surgical procedure.
Tschut (Khat). Propranolol.
- What is Khat?
- How does Khat work?
- Dosing considerations for Khat.
- Are there safety concerns?
- Depression, fatigue, obesity, stomach ulcers, elevating mood, and other uses.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96538
Buy 20 mg propranolol amex
Traumatic injury to the small intestine that leads to fistula formation often occurs from an inside supply physioex 90 cardiovascular physiology generic 40mg propranolol visa, corresponding to a swallowed fish bone blood vessels grow into cornea purchase propranolol 80mg with mastercard, toothpick cardiovascular disease from fast food generic propranolol 80 mg mastercard, magnet, or metallic object. Erosion of these objects into an adjacent loop of small gut leads to an inner enteroenteric fistula. Major penetrating trauma with out damage-control laparotomy rarely results in fistula formation as a outcome of these instances are explored surgically and the intestinal injuries repaired. Patients handled with damage-control laparotomy techniques have an elevated risk for delayed formation of intestinal fistulas caused by extended publicity and desiccation of multiple intestinal loops. An abscess or invasive intestinal infection may erode by way of the gut and create a fistula. Amebiasis, tuberculosis, coccidioidomycosis, actinomycosis, and salmonellosis could trigger intestinal fistulas. Intestinal perforation at the ileum from tuberculosis and typhoid fever continues to be sometimes seen within the Third World. Perforation of the intestinal wall by tumor, inflammation, or operative injury may outcome in the local formation of an abscess. A fistula may develop if this abscess subsequently erodes into an adjoining structure. They also arise from exposure of the bowel to an belly defect or prosthetic mesh used to restore such defects. Abdominal wall dehiscence with evisceration and strangulation of a hernia with infarction and perforation have been implicated within the growth of external fistulas. Fistulas may develop because of percutaneous drainage of an intraabdominal abscess. The small gut and an adjoining structure can become densely adherent from persistent inflammatory circumstances, stomach radiation damage, or tumor erosion. Inflammatory bowel illness, notably Crohn disease, is well-known to create fistulas on this style. In Crohn illness the illness makes fistula formation after anastomosis more likely. Although a spontaneous external fistula can develop as a direct results of Crohn illness, most happen solely after a earlier operation has caused the affected intestine to adhere to the stomach wall. Postoperative fistulas within the setting of Crohn illness are as prone to develop after easy exploration, bypass, or appendectomy as after primary resection. Fistula formation after laparotomy is normally an early complication, especially when arising from an anastomosis, whereas a late fistula typically signifies recurrent Crohn disease. Fistula formation is particularly apt to happen after irradiation of a pelvic malignant lesion. Fistulas that come up secondary to radiation injury hardly ever, if ever, close spontaneously. The tendency for potential injuries should be recognized and overcome, particularly throughout extended laparoscopic instances. A gastrointestinal fistula can be apparent in some patients and intensely difficult to identify in others. Fistula formation is regularly heralded by fever and stomach pain till gastrointestinal contents discharge by way of an stomach incision. Spontaneous fistulas from neoplasm or inflammatory disease usually develop in a extra indolent method. The drainage fluid is often typical of intestinal contents, with obvious bile staining, and intestinal gas may accompany the effluent. At occasions the initial fistula drainage might seem clear rather than yellow or green, and the fistula may be misdiagnosed as a seroma or wound infection. At different times a heavy purulent component may masks the enteric communication and as an alternative recommend a wound an infection. If the drainage persists and the prognosis is uncertain, the patient could also be given activated charcoal or indigo carmine by mouth and the drainage inspected for these substances. The diploma of volume loss and electrolyte imbalance is dependent upon the anatomic location of the fistula and may exceed 3000 mL/day. The commonest abnormalities seen are hypovolemia, hypokalemia, and metabolic acidosis. Hypokalemia occurs primarily from potassium loss in the fistula effluent; hypovolemia contributes by causing renal retention of sodium in change for potassium secretion. Sepsis contributes to the hypovolemic state by elevating the metabolic price and rising insensible water loss. Metabolic acidosis results from the lack of pancreatic juice wealthy in bicarbonate and is extra frequent with proximal fistulas. Gastric fistulas could trigger a hypokalemic, hypochloremic metabolic alkalosis secondary to the loss of a giant quantity of hydrochloric acid. Patients with fistulas inflicting fluid and electrolyte abnormalities have the next mortality rate. Advances in crucial care, invasive monitoring, and aggressive fluid and electrolyte administration can scale back this early mortality significantly, as evidenced by knowledge from the Massachusetts General Hospital. Typically the name of a fistula is derived from the involved and connected organs or buildings. The anatomy of a fistula will recommend the cause and help to predict whether or not spontaneous closure will occur. Fistulas can be categorised physiologically by method of output over a 24-hour period. They may be categorized as low (<200 mL/day), reasonable (200 to 500 mL/day), and high (>500 mL/day). The anatomic and etiologic factors are extra necessary in predicting spontaneous closure than the precise output of the fistula. The underlying illness course of helps to forecast both the closure price and mortality. In distinction, internal fistulas that communicate between the intestine and one other hole viscus is probably not suspected for some time because the symptoms could additionally be minimal or mimic the underlying illness process. Protein�calorie malnutrition and mineral and micronutrient depletion develop in nearly all patients with a small intestinal fistula when an in depth absorptive surface is bypassed or enteric contents are lost externally. Luminal nutrients enhance mucosal cell sloughing and supply native nutrition to the enterocytes. Nutrients in the intestine lumen also have trophic results, similar to growing gastrointestinal hormone and growth issue release that then stimulate the paracrine, endocrine, and autocrine effects of the expansion elements. Indirect effects of intraluminal vitamins embrace increasing motility and gastrointestinal secretions. Magnesium, selenium, and zinc depletion are frequent in sufferers with high-output fistulas and must be monitored. Nutritional deficiencies are worsened by the increased metabolic calls for of sepsis or additional surgical procedure. Abdominal sepsis could result in bacteremia, native and distant infection, and multisystem organ failure. Local extension typically results in wound infection and abdominal wall defects predispose the patient to further sepsis episodes and a excessive mortality rate. The digestive results of the gastrointestinal secretions, particularly pancreatic enzymes, end in appreciable patient discomfort.
Generic 20 mg propranolol free shipping
It is mostly outlined by elevated intraductal pressures on manometric evaluation syndrome x cardiovascular disease order propranolol 80 mg without a prescription. This classification system has been largely abandoned in the trendy era capillaries have generic propranolol 20 mg with mastercard, given newer medical outcomes research cardiovascular system general anatomy purchase propranolol 40 mg with visa. Patients previously designated as sort I often have organic stenosis and are handled with sphincterotomy. Historically, many elaborate exams of the elusive sphincter of Oddi have been described. In the Nardi take a look at (morphineprostigmine provocation test), the patient is administered morphine and neostigmine, and then evaluated for ache or elevated liver or pancreatic serum biochemistries. Biliary scintigraphy can consider for delayed hepatic hilum to duodenum transit time of the nuclear medication tracer, correlating with ampullary obstruction. In basic, these tests are of variable accuracy because of operator inconsistencies. A small-caliber (typically 5 French) multilumen perfusion catheter with an aspiration port is used for stress monitoring. Abnormal pressures could be localized to the pancreatic duct, the bile duct, or may be current in each. Pancreatitis is minimized by use of an aspiration port and by limiting perfusion time and pressure. Endoscopic transpapillary stenting has been undertaken but is generally averted as a end result of excessive danger of pancreatitis. Smooth muscle�relaxing agents such as nifedipine, phosphodiesterase inhibitors, trimebutine, hyoscine butylbromide, and nitric oxide have been used, although without knowledge to present long-term enchancment. Alternative strategies of ache management, including amitriptyline and duloxetine in addition to electroacupuncture, biofeedback, and use of transcutaneous electrical nerve stimulation have also been described. Successful ache aid is achieved in 55% to 95% of patients after this intervention, depending on patient selection. The authors discovered that sphincterotomy was not higher than sham in reducing incapacity because of ache in these patients. The duodenotomy is closed obliquely with a running 3-0 absorbable monofilament suture. In the modern period, ache aid rates in extra of 60% may be anticipated on long-term follow-up after operative transduodenal sphincteroplasty with pancreatic septoplasty. In these patients crucial component of the analysis is a correct history. Laboratory evidence with irregular biliary or pancreatic serum biochemistries, notably during a ache exacerbation episode, is sought. These patients are properly treated with operative transduodenal sphincteroplasty with pancreatic septoplasty. With correct patient selection, long-term pain reduction is predicted in 85% of sufferers. The efficacy of endoscopic sphincterotomy after cholecystectomy in patients with sphincter-of-Oddi dysfunction. Efficacy of endoscopic sphincterotomy and surgical sphincteroplasty for sufferers with sphincter of Oddi dysfunction: randomized, managed examine. A beneficiant Kocher maneuver is used to fully mobilize the duodenum and convey it up into the operative subject. The duodenum and head of pancreas are assessed, noting signs of chronic pancreatitis, which may portend a poor prognosis for postoperative reduction of symptoms. A fibrotic ampulla may be palpable by way of the duodenal wall and may help to guide the location of the duodenotomy. An oblique duodenotomy is made overlying the estimated location of the ampulla using electrocautery. The ampulla is sought throughout the duodenum, with care taken not to traumatize the duodenal mucosa. The needle-tipped cautery is used to make a generous sphincterotomy, dividing the duodenal mucosa and sphincter on prime of the lacrimal duct probe. The pancreatic duct is then sought and cannulated with a separate lacrimal duct probe. The septum between the bile duct and pancreatic duct is split using electrocautery. They are becoming more and more recognized, and extra goal technique of analysis have turn out to be available over the previous two decades. However, significant controversy still stays regarding their best evaluation and therapy. A statistical research of eight hundred and eighty-eight instances of biliary tract disease. Measurement of gallbladder emptying sequentially using a single dose of 99mTclabeled hepatobiliary agent. Surgical remedy for biliary dyskinesia: a metaanalysis and review of the literature. Pilot randomized managed trial of laparoscopic cholecystectomy vs active non-operative remedy for the therapy of biliary dyskinesia. Manometry primarily based randomised trial of endoscopic sphincterotomy for sphincter of Oddi dysfunction. Transduodenal sphincteroplasty in the administration of sphincter of Oddi dysfunction and pancreas divisum in the modern era. Lodhia Irving Waxman ince the first endoscopic visualization and cannulation of the major papilla with cholangiopancreatogram was completed in 1968, rapid advances in the area of endoscopy have elevated the capabilities of physicians to detect, classify, and extra lately, present therapy to disease involving the pancreaticobiliary system. New instruments, equipment, and stents proceed to develop providing access to varied intraabdominal fluid collections or gastrointestinal tract and organs. In pancreaticobiliary circumstances the place tissue acquisition may be limited, enhanced endoscopic-based imaging modalities similar to confocal laser endomicroscopy, contrast-enhanced ultrasonography, and elastography could assist in prognosis and, in certain circumstances, be accepted as surrogates for histologic analysis. While laparoscopic cholecystectomy has since turn out to be the usual, accepted, and most well-liked method for the remedy of gallbladder stones (due to less postoperative pain, lowered hospitalization time, shorter convalescence, and better cosmetic results than open cholecystectomy), laparoscopic management of frequent duct stones is significantly more complex. Advanced surgical skills and complicated instrumentation are required, and neither widely obtainable. The speedy and dramatic enhance in novel endoscopic technology has permitted much less invasive diagnostic and therapeutic maneuvers within the pancreatic and bile ducts that had beforehand required open surgical and percutaneous strategies. Stone retrieval wire baskets with totally different configurations, length/width, kinds of wire, and variety of wires are commercially obtainable. Settings during which a basket may be most well-liked over a balloon include larger stones (>10 mm), intrahepatic stones, smaller stones in a dilated duct, and stones which are bigger than the downstream duct. The emergency mechanical lithotripsy might enable a rescue of the impacted basket; however, surgical procedure could additionally be required to remove the basket. In experienced facilities, frequent duct stones may be successfully removed in 80% to 90% of sufferers after sphincterotomy with normal baskets and balloon catheters. Difficulty clearing or failure to clear the common duct of stones may happen for a wide selection of reasons. Stones larger than 15 mm are typically thought of massive; equally essential, nonetheless, are stone components (such as quantity, consistency, shape, and location) and ductal components (such as contour, diameter on the degree of and distal to the stone, and the presence of coexisting pathology such as a stricture or tumor).

Cheap propranolol 20 mg otc
Exclude a distal obstruction and thoroughly consider areas that have skilled radiation cardiovascular vessels buy generic propranolol 40 mg online, peritonitis cardiovascular disease zucchini buy 80 mg propranolol amex, and native changes (including swelling cardiovascular and cardiothoracic surgeon discount propranolol 20 mg on-line, fistula, inflammatory-based disease and cancer). Precisely dissect tissues included within the anticipated stapling to avoid incorporating extraneous, vascular, or necrotic-prone tissue. Use adequate compression to cause hemostasis and forestall leakage, but avoid excessive compression leading to tissue injury. Stapler configuration/choice may need to be adjusted even within the identical organ when multiple firings are indicated (especially the stomach). This allows for more accurate formation of staples and more steady and hemostatic configuration. Wrapping omentum around an intestinal anastomosis to reinforce the anastomosis and foster the natural means of therapeutic theoretically allows the omentum to mechanically seal the anastomosis in adhesions and play a role in angiogenesis. Tissue adhesives are fibrin glues which might be generally used for hemostasis, bone sealing, and other straightforward tissue repairs. They rely on the conversion of fibrinogen to cross-linked fibrin to aid in hemostasis and the reinforcement of tissue power. In conclusion, the routine clinical use of tissue adhesives for the reinforcement of bowel anastomoses has to be made with consideration. Adhesion limitations are hyaluronic acid�based absorbable movies whose objective is to cut back adhesion formation in the course of the regular therapeutic process. They mechanically separate adhesiogenic tissue by changing into a hydrated gel after which absorbing over the course of approximately every week. Use of a hyaluronic acid�based film has been shown to improve the speed of fistula formation and peritonitis in sufferers undergoing intestinal anastomosis. Furthermore, in a subgroup of patients who had the movie wrapped around a recent anastomosis, anastomotic leak, fistula, peritonitis, abscess, and sepsis occurred significantly more incessantly. In 1985 a biofragmentable anastomotic ring was developed with the intention to facilitate sutureless intestinal anastomosis. The system consists of two similar circular rings composed of Dexon and 12% barium sulfate. Prolene sutures are used to create purse-string stitches at the two cut ends of the bowel, and the sutures are tightened around the rings after the rings are positioned inside the bowel lumens. Further study has proven this gadget to be protected to be used additionally in emergency anastomosis. Both of these devices probably need long-term follow-up earlier than they are going to be thought-about in scientific practice for replacement of traditional anastomotic strategies. Animal research using a bovine pericardium patch to reinforce intestinal anastomosis have proven promising results. Use of a porcine mannequin indicates the patch is safe and effective and demonstrated improvement in mitochondrial function and normalization of mucosal transport after wrapping the anastomosis with the patch. Although these results are promising, future research will have to concentrate on human outcomes before either patch can enter routine scientific follow. Early results point out no significant distinction by method of consequence, leak fee, or an infection for sufferers with intestinal anastomosis. Enhanced intestinal anastomotic therapeutic with gelatin hydrogel incorporating fundamental fibroblast growth issue. Laparoscopic gastrointestinal anastomoses using knotless barbed sutures are protected and reproducible: a single-center experience with 201 sufferers. The hand-sewn anastomosis with an absorbable bidirectional monofilament barbed suture Stratafix throughout laparoscopic one anastomosis loop gastric bypass. Bacterial adherence to surgical sutures: can antibacterial-coated sutures scale back the danger of microbial contamination The impact of various suture supplies on the security of colon anastomosis in an experimental peritonitis mannequin. Single-layer continuous colon and rectal anastomosis utilizing monofilament absorbable suture (Maxon). Single- versus two-layer intestinal anastomosis: a meta-analysis of randomized managed trials. Single layer versus double layer suture anastomosis of the gastrointestinal tract. A managed trial of inverting versus everting intestinal suture in scientific large-bowel surgery. The use of staplers in anatomical side-to-side and useful end-to-end enteroanastomoses. The ideal time to resume oral feeding after intestinal anastomosis has been the topic of a lot debate. The preponderance of evidence points to the dearth of hurt, and sometimes the profit, of early oral feeding. Despite their articulation and the appreciated importance of a selection of preoperative and postoperative maneuvers, the best method seems to vary by location, affected person elements, general context, and surgeon perspective, talent, and expertise. Because of the biology involved in this activity, the creation of an anastomosis stays one thing of an art kind. Anastomotic leak will increase distant recurrence and long-term mortality after healing resection for colonic most cancers. Reducing gastrointestinal anastomotic leak charges: review of challenges and solutions. Surgical stapling device�tissue interactions: what surgeons must know to improve patient outcomes. Effects of physical configuration and chemical structure of suture materials on bacterial adhesion. Profiling surgical staplers: impact of staple height, buttress, and overlap on staple line failure. Effect of an omental wrap on the healing and vascularity of compromised intestinal anastomoses. Omentoplasty within the prevention of anastomotic leakage after colonic or rectal resection. Adverse influence of fibrin sealant on the therapeutic of high-risk sutured colonic anastomoses. Effects of hyaluronic acidcarboxymethylcellulose antiadhesion barrier on ischemic colonic anastomosis. A prospective, randomized, multicenter, controlled study of the security of Seprafilm adhesion barrier in abdominopelvic surgery of the gut. Comparison of the Valtrac biofragmentable anastomosis ring with conventional suture and stapled anastomosis in colon surgery. Bovine pericardium patch wrapping intestinal anastomosis improves therapeutic process and prevents leakage in a pig mannequin. Intra-abdominal drains for the prophylaxis of anastomotic leak in elective colorectal surgery. Factors associated with the prevalence of leaks in stapled rectal anastomoses: a review of 1,014 patients.
Purchase 40 mg propranolol with amex
Clinical Gastroenterology and Hepatology: the Official Clinical Practice journal of the American Gastroenterological Association blood vessels growing over cornea discount 20mg propranolol with amex. A nasocystic catheter and two double pigtails (or metallic stents to create a larger and extra completely "supported" opening to the cavity) are placed in the collection arteries location generic 80mg propranolol mastercard, to be used for flushing the contents into the abdomen or duodenum (1 L per 24 hours) heart disease kills more than cancer purchase 80 mg propranolol. Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by international consensus. International Association of Pancreatology/American Pancreatic Association evidence-based pointers for the management of acute pancreatitis. Extrapancreatic necrosis with out pancreatic parenchymal necrosis: a separate entity in necrotising pancreatitis A conservative and minimally invasive method to necrotizing pancreatitis improves end result. Organ failure and an infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Persistent organ failure in the course of the first week as a marker of deadly consequence in acute pancreatitis. Association between early systemic inflammatory response, severity of multiorgan dysfunction and demise in acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 by way of 13, 1992. Update on acute pancreatitis: ultrasound, computed tomography, and magnetic resonance imaging features. Prediction of mortality in acute pancreatitis: a scientific evaluate of the printed proof. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. Faster price of preliminary fluid resuscitation in severe acute pancreatitis diminishes in-hospital mortality. Early fluid resuscitation reduces morbidity among sufferers with acute pancreatitis. Rapid hemodilution is related to elevated sepsis and mortality amongst patients with extreme acute pancreatitis. Randomized clinical trial of specific lactobacillus and fibre supplement to early enteral vitamin in patients with acute pancreatitis. Synbiotic control of irritation and infection in extreme acute pancreatitis: a prospective, randomized, double blind study. Probiotic prophylaxis in predicted extreme acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Antibiotic therapy for prophylaxis towards an infection of pancreatic necrosis in acute pancreatitis. Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Controlled medical trial of selective decontamination for the treatment of extreme acute pancreatitis. Effect of selective decontamination on antimicrobial resistance in intensive care units: a systematic evaluation and meta-analysis. Gastrointestinal motility and gastric tube feeding in mechanically ventilated sufferers. Nutritional approach in malnourished surgical patients: a prospective randomized examine. Management of diet in European intensive care items: outcomes of a questionnaire. Working group on metabolism and diet of the European Society of Intensive Care Medicine. Intestinal hypoperfusion contributes to intestine barrier failure in severe acute pancreatitis. Bacterial translocation and infected pancreatic necrosis in acute necrotizing pancreatitis derives from small bowel rather than from colon. Early endoscopic retrograde cholangiopancreatography in predicted severe acute biliary pancreatitis: a prospective multicenter research. Lack of consensus on the position of endoscopic retrograde cholangiography in acute biliary pancreatitis in published meta-analyses and tips: a scientific review. Systematic review of percutaneous catheter drainage as main therapy for necrotizing pancreatitis. Efficacy of conservative treatment, with out necrosectomy, for contaminated pancreatic necrosis: a systematic review and meta-analysis. Feasibility of minimally invasive approaches in patients with infected necrotizing pancreatitis. Management of infected pancreatic necrosis utilizing retroperitoneal necrosectomy with flexible endoscope: 10 years of expertise. Three-port retroperitoneoscopic necrosectomy in administration of acute necrotic pancreatitis. Treatment of severe acute pancreatitis by way of retroperitoneal laparoscopic drainage. Endoscopic ultrasound-guided versus conventional transmural drainage for pancreatic pseudocysts: a prospective randomized trial. Non-fluoroscopic endoscopic ultrasound-guided transmural drainage of symptomatic non-bulging walled-off pancreatic necrosis. Preliminary report on a new, fully lined, metal stent designed for the treatment of pancreatic fluid collections. Factors impacting treatment outcomes in the endoscopic management of walled-off pancreatic necrosis. Dual-modality drainage of contaminated and symptomatic walled-off pancreatic necrosis: long-term clinical outcomes. Outcomes after implementing a tailor-made endoscopic step-up strategy to walled-off necrosis in acute pancreatitis. Interventions for necrotizing pancreatitis: abstract of a multidisciplinary consensus convention. Diagnostic technique and timing of intervention in contaminated necrotizing pancreatitis: an international expert survey and case vignette examine. Clinical views in pancreatology: compliance with acute pancreatitis tips in Germany. Appropriate timing of cholecystectomy in sufferers who present with average to extreme gallstone-associated acute pancreatitis with peripancreatic fluid collections. The function of routine fine-needle aspiration within the diagnosis of contaminated necrotizing pancreatitis.
Discount propranolol 80 mg amex
Efficacy and safety of imatinib mesylate in superior gastrointestinal stromal tumors arteries carry oxygenated blood purchase propranolol 40 mg without prescription. Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1 type 1 capillaries order 20 mg propranolol free shipping,640 sufferers cardiovascular systems inc stock propranolol 40mg online. Discontinuation of imatinib in sufferers with superior gastrointestinal stromal tumours after three years of treatment: an open-label multicentre randomised section 3 trial. Clinical efficacy of second-generation tyrosine kinase inhibitors in imatinib-resistant four. Underreporting of gastrointestinal stromal tumors: is the true incidence being captured Validation of the Joensuu danger criteria for primary resectable gastrointestinal stromal tumour- the influence of tumour rupture on affected person outcomes. Development and validation of a prognostic nomogram for recurrence-free survival after full surgical resection of localised major gastrointestinal stromal tumour: a retrospective evaluation. Microscopically optimistic margins for primary gastrointestinal stromal tumors: evaluation of threat factors and tumor recurrence. Surgical administration and medical outcome of gastrointestinal stromal tumor of the colon and rectum. Comparison of the post-operative outcomes and survival of laparoscopic versus open resections for gastric gastrointestinal stromal tumors: a multi-center potential cohort study. Furthermore, upon laparotomy, the bowel lesion had to be proven to be dominant, and only involvement of lymph nodes in the quick neighborhood of the first lesion was acceptable. Patients have been excluded from analysis when distant stomach lymph nodes, spleen, or liver had been concerned. Histologically, tumors encompass diffuse sheets of large, blastic lymphoid cells, 2 to four occasions larger than normal lymphocytes, usually infiltrating and destroying the gastric glandular architecture. Lymphoid follicles develop in the presence of continual inflammation and gastritis related to H. In basic, a specialist in hematology or medical oncology is the "quarterback" of the multidisciplinary group managing these sufferers. This technique of nonsurgical administration has been established in two randomized managed trials evaluating the position of surgical procedure within the management of early Lugano system (Table 82. Perhaps the worst outcome in patients present process major resection is the occasional patient who incurs critical postoperative problems similar to intraabdominal abscess, enterocutaneous fistula, prolonged sepsis, and inanition, which significantly delay or impair the delivery of sufficient chemoimmunotherapy. If a lymphoma is confirmed, the surgeon must make a decision about whether or not to proceed with the planned resection. In common, if a safe, low-risk resection will take away all grossly concerned bowel, this is ready to be the preferred course; however, if the surgical procedure is nonemergent and resection can be complicated, high-risk, multivisceral, and/or embrace main vascular resection, it must be prevented and the procedure terminated after enough tissue for diagnostic studies is obtained. The radiology analysis was angiosarcoma, however this proved to be a diffuse large B-cell lymphoma. Routine surgical pathology including evaluation of frozen section and fixed hematoxylin and eosin sections which, mixed with medical correlation (site of presentation, age, predisposing factors), present a tentative diagnosis. These checks set up the cell lineage and monoclonality of the abnormal cell population and confirm or modify the initial pathologic diagnosis. When a surgeon resects tissue in a known or suspected case of lymphoma, communication with the pathologist on obligation is essential to ensure that enough tissue is obtained and dealt with correctly to enable the complete vary of diagnostic testing. In reality, the explosion of new agents has opened up a frightening number of potentialities for future analysis,49 which is in a position to take some time to come into focus. Although a complete dialogue is past the scope of this chapter, the following will present a present overview for the reader, who can also be referred to a quantity of current evaluations on these subjects. Cyclophosphamide and fludarabine are also administered as conditioning chemotherapy. Despite this, nine patients remained in ongoing remission finally follow-up, with the longest remission at 23 months from remedy. The conditioning routine various relying on the histologic subtype and previous treatment historical past. Management of major gastrointestinal non-Hodgkin lymphomas: a population-based survival evaluation. Enteropathy-type T-cell lymphoma: clinical options and treatment of 31 patients in a single establishment. Survival in refractory celiac disease and enteropathy-associated T-cell lymphoma: retrospective analysis of single-centre expertise. Enteropathy-associated T-cell lymphoma: clinical and histological findings from the international peripheral T-cell lymphoma project. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Idelalisib, a selective inhibitor of phosphatidylinositol 3-kinase-delta, as remedy for previously treated indolent non-Hodgkin lymphoma. Primary gastrointestinal lymphoma: spectrum of imaging findings with pathologic correlation. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Primary gastrointestinal lymphoma in Japan: a clinicopathologic evaluation of 455 patients with particular reference to its time developments. Lymphoma/leukemia molecular profiling project: the utilization of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. Bcl-6 protein expression, and not the germinal centre immunophenotype, predicts beneficial prognosis in a collection of primary nodal diffuse giant B-cell lymphomas: a single centre expertise. Survival prediction of diffuse large-B-cell lymphoma based mostly on both clinical and gene expression data. Chromosomal translocation t(11;18)(q21;q21) in gastrointestinal mucosa associated lymphoid tissue lymphoma. Report on a workshop convened to talk about the pathologic and staging classification of gastrointestinal tract lymphoma. The role of surgery in primary gastric lymphoma: results of a managed medical trial. Survival of patients with marginal zone lymphoma: analysis of the survival, epidemiology, and end-results database. Congenital lesions, similar to rotational anomalies, duodenal or jejunoileal atresia, meconium ileus, omphalomesenteric remnants, and duplication cysts, are more likely to present in infancy, if not prenatally. Although 90% of circumstances manifest during the first 12 months of life (with 50% to 75% presenting within the first month of life),1 patients might present with midgut volvulus and/or obstruction at any age, making an understanding of the embryology, analysis, and therapy of malrotation important for all stomach surgeons. At week 10, the midgut returns to the abdomen, rotating another one hundred eighty levels counterclockwise. The right and left colons are anchored to the posterior belly wall by mesenteric attachments. In addition, Ladd bands extending from the best paracolic region to the malpositioned cecum could obstruct the duodenum. Congenital diaphragmatic hernias and belly wall defects (omphaloceles and gastroschisis) intervene with or abrogate normal rotation earlier than the 10th week of gestation; as such, infants with these conditions are malrotated by definition.
References
- International Agency for Research on Cancer. Smokeless Tobacco and Tobacco-Specific Nitrosamines. Vol 89.
- Fuchs J, Szavay P, Seitz G, et al: Nephron sparing surgery for synchronous bilateral nephroblastoma involving the renal hilus, J Urol 186:1430n1436, 2011.
- Rihal CS, Naidu SS, Givertz MM, et al. 2015 SCAI/ACC/HFSA/STS clinical expert consensus statement on the use of percutaneous mechanical circulatory support devices in cardiovascular care: Endorsed by the American heart assocation, the cardiological society of India, and sociedad latino Americana de cardiologia intervencion; affirmation of value by the Canadian association of interventional cardiologyassociation Canadienne de cardiologie d'intervention. J Am Coll Cardiol. 2015;65:e7-e26.
- Shiran A, Sagie A. Tricuspid regurgitation in mitral valve disease. jAm Con Cardfol. 2009;53:4() 1-4<>8.
- Martin D, Pascal J, Baudet J, et al. The submental island flap: a new donor site. Anatomy and clinical applications as a free or pedicled flap. Plast Reconstr Surg 1993;92:867-873.