Clarinex
Linda M. Dairiki Shortliffe, MD
- Stanley McCormick Memorial Professor and Chair,
- Department of Urology, Stanford University School of
- Medicine
- Chief of Urology, Stanford University Medical
- Center
- Chief of Pediatric Urology, Lucile Salter Packard
- Children’s Hospital, Stanford, California
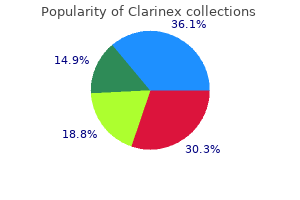
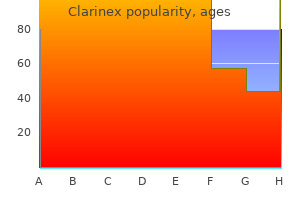
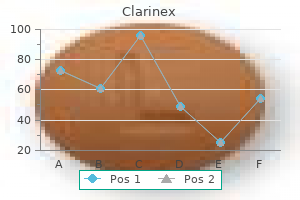
Clarinex dosages: 5 mg
Clarinex packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Effective clarinex 5 mg
Rayes N best allergy medicine for 5 yr old discount 5mg clarinex visa, et al: Effect of enteral nutrition and synbiotics on bacterial infection rates after pylorus-preserving pancreatoduodenectomy: a randomized allergy medicine for adults discount clarinex 5 mg with mastercard, double-blind trial allergy symptoms nose clarinex 5 mg overnight delivery, Ann Surg 246(1):36�41, 2007. Richter B, et al: Nutritional help after open liver resection: a scientific evaluation, Dig Surg 23(3):139�145, 2006. Sadamori H, et al: Risk elements for organ/space surgical website an infection after hepatectomy for hepatocellular carcinoma in 359 recent cases, J Hepatobiliary Pancreat Sci 20(2):186�196, 2013. Scilletta R, et al: Comparative evaluation of the incidence of surgical site infections in patients with liver resection for colorectal hepatic metastases after neoadjuvant chemotherapy, J Surg Res 188(1):183� 189, 2014. Shinkawa H, et al: Nutritional threat index as an impartial predictive factor for the development of surgical website an infection after pancreaticoduodenectomy, Surg Today 43(3):276�283, 2013. Springer R: the Surgical Care Improvement Project-focusing on an infection control, Plast Surg Nurs 27(3):163�167, 2007. Stewart L, et al: Antibacterial exercise of bile acids towards common biliary tract organisms, Surg Forum 37:157�159, 1986. Su Z, et al: Factors influencing infectious problems after pancreatoduodenectomy, J Hepatobiliary Pancreat Sci 17(2):174�179, 2010. Sudo T, et al: Perioperative antibiotics covering bile contamination stop stomach infectious problems after pancreatoduodenectomy in patients with preoperative biliary drainage, World J Surg 38(11):2952�2959, 2014. Sugiura T, et al: Risk issue of surgical web site an infection after pancreaticoduodenectomy, World J Surg 36(12):2888�2894, 2012. Effects of hydrophobicity of the molecule and in the presence of phospholipids, Dig Dis Sci 38(11):2104�2112, 1993. Suzuki Y, et al: Randomized clinical trial of preoperative intranasal mupirocin to cut back surgical-site infection after digestive surgical procedure, Br J Surg 90(9):1072�1075, 2003. Togo S, et al: Perioperative infection control and its effectiveness in hepatectomy patients, J Gastroenterol Hepatol 22(11):1942�1948, 2007. Togo S, et al: Usefulness of absorbable sutures in stopping surgical website infection in hepatectomy, J Gastrointest Surg 12(6):1041�1046, 2008. Uchiyama K, et al: Risk factors for postoperative infectious problems after hepatectomy, J Hepatobiliary Pancreat Sci 18(1):67�73, 2011. Van Buren G 2nd, et al: A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage, Ann Surg 259(4):605�612, 2014. Wang A, et al: Analysis of surgical web site infection rate in pancreas operation and its associated danger elements, Zhongguo Yi Xue Ke Xue Yuan Xue Bao 29(4):562�565, 2007. Watanabe F, et al: Risk elements for intra-abdominal an infection after pancreaticoduodenectomy-a retrospective analysis to consider the significance of preoperative biliary drainage and postoperative pancreatic fistula, Hepatogastroenterology 59(116):1270�1273, 2012. Yanaga K, et al: Intraperitoneal septic issues after hepatectomy, Ann Surg 203(2):148�152, 1986. Yang T, et al: Risk elements of surgical site an infection after hepatic resection, Infect Control Hosp Epidemiol 35(3):317�320, 2014. With the ease and availability of refined high-resolution scanning, there would possibly develop a bent for the physician to "scan first, clinic later," and this have to be averted. A thorough scientific evaluation will information the appropriateness and use of additional checks and must embrace a careful balancing of potential risk versus good factor about any investigation or intervention in any specific individual, depending on their health, comorbidity, and personal or household needs. Accurate recording of alcohol consumption should be made, as a result of ongoing heavy alcohol use impacts therapy for chronic liver or pancreatic illnesses. Occasionally, sufferers attend the clinic smelling of alcohol of their breath, but deny ongoing alcohol use, and this must be famous. A request for a blood alcohol stage might be made, provided the affected person consents to it. A previous medical history ought to be obtained to embrace any major sicknesses and any stomach surgery. A document of comorbidities and exercise tolerance ought to be made, as it will information the surgeon in assessing health for future intervention if required (see later). This ought to be adopted by a household historical past, drug history, social circumstances, employment, and travel. Abdominal ache is commonly a presenting symptom, and a detailed enquiry of the location, severity, radiation, and rapidity of onset will permit some clues to a differential diagnosis. Suddenonset severe upper stomach ache radiating to the back is characteristic of acute pancreatitis (see Chapters 55 and 56), whereas right-side upper quadrant ache might indicate acute irritation of the gallbladder (see Chapter 33). Any related nausea and vomiting ought to be recorded along with a historical past of jaundice (sclerae), color of urine and stools, and any associated itching. A historical past of stomach distension may level to an ileus in acute presentations and to ascites or bowel obstruction in continual liver illness or a malignant process. Steatorrhea is characterised by the passage of foul-smelling stools, which float on water and may point out pancreatic exocrine insufficiency (see Chapters fifty seven, fifty eight, and 62). Full publicity of the stomach in good light is essential for an enough inspection. Particular attention ought to be paid to any scars from earlier stomach surgical procedure, stomach distension, and areas of discoloration. Palpation of the abdomen ought to start with a common mild palpation, on the lookout for apparent masses or areas of tenderness. The healthy liver is often impalpable; nevertheless, in very thin people, the anterior edge may be palpable. A lobe could endure hypertrophy and become palpable, and this may occur in the presence of hemiliver atrophy or after liver resection. Reduction in liver dimension is also important as a end result of this will occur in cirrhosis and certain types of hepatitis. Rotation of the patient forty five levels to the proper could assist palpation, because the spleen then falls onto the analyzing right hand. During this maneuver, the left hand should help the rib cage and loosen up the pores and skin and stomach musculature by drawing these right down to the proper. Percussion may be helpful, and if ascites is present, the spleen may be ballotable. If the spleen is sufficiently enlarged, the notch on its anterior border could turn into palpable. The liver is examined using a combination of palpation and percussion from above and beneath to delineate its borders. Dullness to percussion of the higher border extends so far as the fifth intercostal house. Auscultation can additionally be important as a result of a venous hum could additionally be heard with portal hypertension, and a bruit may be heard in association with hepatocellular carcinomas. Portal Hypertension Portal hypertension is as a outcome of of both intrahepatic or extrahepatic portal venous obstruction (see Chapters 76 and 79). The extra widespread medical website of portosystemic anastomosis is at the gastroesophageal junction, leading to esophageal varices; any evidence of upper gastrointestinal blood loss, whether hematemesis or melena, ought to be investigated with urgent endoscopy. Extrahepatic portal hypertension is usually due to portal vein thrombosis, and as such it is important to establish any history of neonatal infection around the umbilicus, main intraabdominal sepsis or pancreatitis, pancreatic cancer, or a blood disorder that might lead to hypercoagulability.
Purchase 5mg clarinex mastercard
Sun S allergy forecast sacramento cheap clarinex 5mg overnight delivery, et al: Three-port versus four-port laparoscopic cholecystectomy: meta-analysis of randomized scientific trials allergy symptoms 2 year old order clarinex 5 mg with amex, World J Surg 33(9):1904� 1908 allergy symptoms 2015 purchase clarinex 5 mg without a prescription, 2009. Svoboda S, et al: Robotic single-site cholecystectomy within the obese: outcomes from a single establishment, Surg Obes Relat Dis 11(4):882� 885, 2015. Tagge E, et al: Impact of laparoscopic cholecystectomy on the administration of cholelithiasis in youngsters with sickle cell illness, J Pediatr Surg 29:209�212, 1994. Tuveri M, Tuveri A: Laparoscopic cholecystectomy: issues and conversions with the 3-trocar approach: a 10-year review, Surg Laparosc Endosc Percutan Tech 17(5):380�384, 2007. Ure B, et al: Long-term results after laparoscopic cholecystectomy, Br J Surg eighty two:267�270, 1995. Open cholecystectomy and bile duct exploration were carried out generally as the usual remedy for patients with choledocholithiasis for a number of years with good success and low rates of morbidity and mortality. During this period of open operative interventions, the percentage of retained stones was only 1% to 3%, and longterm follow-up revealed that revisional surgical procedure was necessary in solely about 10% of the patients. Time constraints and lack of equipment were the main elements preventing the application of the laparoscopic method for treating choledocholithiasis (Bingener & Schwesinger, 2006). Despite these issues, there remain indications for operative choledochotomy and, more specifically, for open exploration. Secondary stones, those who originate within the gallbladder and migrate into the bile duct, are the most typical. This is related to the excessive incidence of intrahepatic bile duct stones seen primarily in Southeast Asian countries, Taiwan, Hong Kong, and Singapore (Kim et al, 1995) (see Chapter 39). The relative prevalence of intrahepatic bile duct stones in all gallstone circumstances in Taiwan is extremely excessive (>50%), and coexisting intrahepatic and extrahepatic bile duct stones are present in roughly 70% of these. Inflammatory, infective, and congenital typical shows of choledocholithiasis embrace biliary colic, jaundice, cholangitis (see Chapter 43), and pancreatitis (see Chapter 55). If untreated for a protracted time frame, these recurrent episodes could lead to secondary biliary cirrhosis. More than one half of patients who had retained bile duct stones experienced recurrent symptoms during a follow-up interval of 6 months to 13 years (Johnson & Hosking, 1987), and 25% developed critical issues (Caddy & Tham, 2006). The potential long-term sequelae of untreated clinically significant stones has led some to advocate for routine intraoperative cholangiography at the time of cholecystectomy in order that clearance of the duct at the time of surgical procedure could be ensured. During the period of open cholecystectomy, the practice of routine cholangiography was common, and research from this era demonstrated an incidence of choledocholithiasis approaching 10% to 15% in patients with none clinically evident frequent duct involvement (Coelho et al, 1984; DenBesten & Berci, 1986; Doyle et al, 1982; Ganey et al, 1986; Girard, 2000; Hampson et al, 1981; Lygidakis, 1983; McSherry & Glenn, 1980). This has brought on some to advocate for the utility of routine intraoperative cholangiography, even in sufferers with out scientific indicators of choledocholithiasis. The use of selective intraoperative cholangiography in laparoscopic cholecystectomy series demonstrates similar findings (Fogli et al, 2009). Collins and colleagues (2004) identified filling defects in maintaining with stones in 4. In these patients, entry was maintained for the performance of postoperative cholangiograms. At 48 hours, 26% of sufferers had a normal cholangiogram, and a further 26% had proof for passage of the stones by 6 weeks. A worth higher than 90 U/L has been proposed to point out a high danger of choledocholithiasis, with sensitivity and specificity of 86% and 74. When used in conjunction, clinical examination, laboratory research, and ultrasonography (typically the first-line imaging modality) (see Chapter 15) are sensitive in 96% to 98% and specific in 40% to 75% for identification of patients with choledocholithiasis (Alponat et al, 1997; Koo & Traverso, 1996; Trondsen et al, 1998). The occurrence of choledocholithiasis in these groups (group 1, extremely excessive risk; group 2, excessive threat; group three, moderate risk; group four, low risk) was ninety two. Using these elements, sufferers are stratified into high, intermediate, and low chance for choledocholithiasis groups. Presence of any "very robust" or both "sturdy" predictors leads to classification as high probability for choledocholithiasis. The sensitivity of this method could be as excessive as 97%, and the specificity is 75% to 96% (Anderson et al, 2008; Cabada Giad�s et al, 2002; Gibson et al, 2005; Kim et al, 2007; Kondo et al, 2005; Maniatis et al, 2003; Polkowski et al, 1999; Soto et al, 2000; Zandrino et al, 2005). A systematic evaluation (Martin et al, 2006) demonstrated that open surgery resulted in less mortality, decrease incidence of main remedy failure, and fewer procedures required per affected person. Given these data, single-stage cholecystectomy and bile duct exploration (as indicated) was the preferred approach within the era of open cholecystectomy. Several potential randomized controlled trials in contrast these two remedy methods (Cuschieri et al, 1999; Rogers et al, 2010; Sgourakis et al, 2005) and found the 2 teams had equivalent success charges of duct clearance and affected person morbidity, however a significantly shorter hospital keep was reported with the single-stage laparoscopic therapy. Treatment strategies for sufferers stratified to the high and low probability teams are typically agreed upon. They famous sufferers who underwent elective open cholecystectomy had considerably fewer recurrent biliary signs (6% vs. In contrast to the final consensus of tips on how to deal with highand low-likelihood sufferers, the question of how to deal with intermediate-risk patients has been the topic of some debate. No significant distinction was present in morbidity or high quality of life; nevertheless, sufferers who underwent cholecystectomy because the initial process had a considerably shorter size of keep (median, 5 days vs. Based on these findings, the authors suggested that initial cholecystectomy with intraoperative cholangiogram could additionally be the preferred strategy. The rate of recurrence will increase to approximately 20% after a second operation on the biliary tract for choledocholithiasis (Saharia et al, 1977; Way, 1973), and this price increases after subsequent reoperation (Allen et al, 1981). Decision making is further influenced by medical presentation, situation of the affected person, institutional expertise, and presence or absence of a T-tube. The rise in recognition of laparoscopic biliary surgery has also meant reducing use of the T-tube. If a T-tube is current, it provides noninvasive choices for accessing the biliary tree postoperatively. Because of its high success rate and low morbidity and mortality, nonoperative mechanical extraction via the T-tube tract is an attractive treatment choice. A success rate of 95% has been reported with a morbidity price of only 4% (Mazzariello, 1978). When complications do occur, they can be handled medically in most instances, and solely 0. In areas of the growing world, nonetheless, the place access to endoscopic, radiologic, and laparoscopic expertise is restricted, open cholecystectomy and bile duct exploration stays a mainstay of remedy. Postcholecystectomy Choledocholithiasis (See Chapter 38) Incidence the majority of initial operations for gallstone disease, with or without demonstrated choledocholithiasis, are healing, but some sufferers will develop sequelae of choledocholithiasis postcholecystectomy. If these techniques fail, operative administration could be undertaken with the expectation of a excessive success rate and acceptable morbidity and mortality (Cameron, 1989; Girard & Legros, 1981). Hemorrhage, pancreatitis, cholangitis, and perforation are essentially the most frequent problems, and mortality usually is reported at zero. Long-term complication charges, primarily from stenosis or new stones or each, are low (<10%), and most complications could be managed endoscopically (Cotton, 1984; Escourrou et al, 1984; Hammarstr�m et al, 1996; Sivak, 1989). In such settings, operative management is the most affordable alternative (Cameron, 1989). Reoperation for retained stones could be performed safely, with operative mortality less than 2% (Girard & Legros, 1981).

Discount 5mg clarinex with mastercard
Most have high-grade dysplasia allergy index nyc purchase 5 mg clarinex with amex, which must be graded on the idea of the most extreme focus allergy shots exercise clarinex 5mg low cost. Adenomas are uncommon within the bile ducts allergy testing wiki buy discount clarinex 5mg, and most exophytic bile duct tumors are collectively designated intraductal papillary neoplasms, together with cases beforehand reported as papillomatosis (Gouma et al, 1984; Sagar et al, 1993; Taguchi et al, 1993). Recently, the biliary counterpart of pancreatic intraductal tubulopapillary neoplasm, intraductal tubular (or tubulopapillary) neoplasm of the bile ducts, has also been described (Katabi et al, 2012; Park et al, 2010; Schlitter et al, 2015; Zen et al, 2012). Cystic dilation of the bile ducts might occur (Zen et al, 2006) and a few instances exhibit mucin hypersecretion (Katabi et al, 2012; Shibahara et al, 2004). However, variations within the frequency and types of related invasive carcinoma, as well as the morphology and immunophenotype, are vital (Klimstra, 2002). Of notice, accumulating data counsel regional geographic variations in the proportion of intraductal papillary neoplasms with the totally different cell types, maybe related to various etiologic elements in several parts of the world (Shibahara et al, 2004). In Asian patients, for example, an affiliation of intraductal papillary neoplasms with Clonorchis an infection has been reported (Jang et al, 2008) (see Chapter 45). Small gallbladder adenomas could display high-grade dysplasia, but invasive carcinomas are very rare. In contrast, intracystic/ intraductal papillary and tubulopapillary neoplasms have related invasive carcinomas in additional than half of all instances (Adsay et al, 2012; Choi et al, 2010; Katabi et al, 2012; Rocha et al, 2012; Schlitter et al, 2015). Most invasive carcinomas arising in these neoplasms are standard tubular (pancreatobiliarytype) adenocarcinomas, similar to different bile duct carcinomas (Adsay et al, 2012; Katabi et al, 2012; Schlitter et al, 2015). Some cases have a mucinous (colloid) sample, normally when the intraductal neoplasm is of the intestinal type. Undifferentiated carcinoma and poorly differentiated neuroendocrine carcinoma have also been reported (Albores-Saavedra et al, 2010). Noninvasive intracystic/intraductal papillary and tubular neoplasms have an excellent prognosis. However, some noninvasive circumstances still follow an aggressive clinical course, doubtless because of missed foci of invasion or a field-effect phenomenon with multicentric biliary neoplasia, and therefore long-term comply with up is really helpful. Interestingly, even those related to an invasive carcinoma have a greater scientific outcome in contrast with typical pancreatobiliary-type biliary carcinomas (Adsay et al, 2012; Albores-Saavedra et al, 2000; Katabi et al, 2012; Rocha et al, 2012; Schlitter et al, 2015). One lesion to be distinguished from intraductal papillary neoplasms of the bile ducts is biliary mucinous cystic neoplasm, also referred to as hepatobiliary cystadenoma (Devaney et al, 1994; Wheeler & Edmondson, 1985;). Biliary mucinous cystic neoplasms are analogous to mucinous cystic neoplasms of the pancreas and are additionally considered a type of mass-forming preinvasive neoplasm. They type multilocular cystic lesions that happen predominantly in adult ladies and exhibit pathognomonic hormone receptor�expressing ovarian-type subepithelial stroma (Grayson et al, 1996). The lining epithelium is com- posed of cuboidal to columnar cells, sometimes with plentiful apical mucin. Although most biliary mucinous cystic neoplasms show benign cytoarchitectural features, some could harbor foci of high-grade dysplasia or invasive carcinoma. Most circumstances are nonfunctioning, and patients are seen with signs and signs of biliary obstruction. Rare examples may be associated with von Hippel�Lindau syndrome (Sinkre et al, 2001). Grossly, well-differentiated neuroendocrine tumors form comparatively well-demarcated nodules and could additionally be polypoid and mucosa lined. Rarely, the cytoplasm may exhibit clear-cell, oncocytic, or signet ring�like modifications. In basic, these tumors are low-grade malignancies with an indolent scientific course. Rarely, paraganglioma (Caceres et al, 2001; Mehra & Chung-Park, 2005), a tumor that additionally shows neuroendocrine differentiation, may occur in the biliary tract. However, for large-cell neuroendocrine carcinomas (Papotti et al, 2000), optimistic immunohistochemical staining for chromogranin or synaptophysin must be obtained to verify the prognosis. Half of small-cell carcinomas are pure, but a significant proportion of large-cell neuroendocrine carcinomas are admixed with standard adenocarcinomas (Maitra et al. However, these tend to be delicate to chemotherapy with platinum-based protocols. These are predominantly seen in kids three to 4 years old and constitute 1% of all rhabdomyosarcomas (see Chapter 95). The tumor consists of a conglomerate of sentimental, mucosa-covered polyps filling the lumen. Beneath the floor layer of flattened biliary epithelium is a dense zone of primitive spindle cells, representing the cambium layer. Cytoplasmic cross-striations may be seen, and skeletal muscle differentiation is demonstrable by immunohistochemical staining for actin, desmin, or myoD1. Although the prognosis is poor, multimodal therapy has resulted in long-term survival in some sufferers. Metastases happen in 40% of patients, however dying usually is caused by the native effects of the tumor. It is characterised by cells containing ample acidophilic granular cytoplasm, often with bigger globules. This tumor is of unsure origin, but most proof, including expression of S-100 protein, indicates a relationship to Schwann cells. Although it has an infiltrative look, granular cell tumor is benign with solely minimal recurrence potential, even when incompletely excised. A variety of other mesenchymal tumors have been documented within the biliary tree, each benign and malignant. Benign tumors embrace hemangioma (Furukawa et al, 1997), lymphangioma (Choi et al, 2002), neurofibroma (Sucandy et al, 2010), schwannoma (Panait et al, 2011), ganglioneuroma (almost at all times related to a quantity of endocrine neoplasia type 2b) (Chetty & Clark, 1993), leiomyoma (Furukawa, 1996), myofibroblastic tumors, lipoma (Furukawa, 1996), and osteoma (Chen, 1994). Malignant mesenchymal tumors embody angiosarcoma (Odashiro et al, 2005), Kaposi sarcoma (Lesman et al, 1993), leiomyosarcoma (Danikas et al, 2001), chondrosarcoma, peripheral nerve sheath tumor (Chang et al, 1997), and malignant fibrous histiocytoma. These tumors are documented largely as case reports (Adsay, 2015; Adsay & Klimstra, 2015; Albores-Saavedra et al, 2000; Lack, 2003). Before a case is classed as sarcoma, the potential of a sarcomatoid carcinoma should be carefully thought of. Secondary Tumors the biliary tree could additionally be involved by a wide selection of carcinomas originating in other organs, particularly the pancreas, abdomen, colon, kidney, and breast, both by metastasis or direct invasion (Adsay, 2015; Adsay & Klimstra, 2015; Albores-Saavedra et al, 2000; Lack, 2003). Among these, metastatic renal cell carcinoma is notorious for mimicking a main tumor as a result of it might kind a polypoid luminal lesion, and the history of the first tumor may be distant. Metastases from main colorectal cancer to the biliary epithelium have additionally been described (Povoski et al, 2000) and can mimic intraductal papillary neoplasms. Primary lymphomas of the mucosa-associated lymphoid tissue type also have been reported. Rarely, heterotopic tissue, especially pancreatic tissue (Cerullo et al, 2011; Mrak et al, 2010), could form a mass.
Effective 5 mg clarinex
Akhurst T allergy shots weekly cheap 5mg clarinex fast delivery, et al: Recent chemotherapy reduces the sensitivity of [18F] fluorodeoxyglucose positron emission tomography in the detection of colorectal metastases allergy medicine edema buy generic clarinex 5mg line, J Clin Oncol 23:8713�8716 allergy shots needle size generic 5mg clarinex visa, 2005. Annunziata S, et al: Diagnostic accuracy of fluorine-18-fluorodeoxyglucose positron emission tomography in the analysis of the first tumor in sufferers with cholangiocarcinoma: a meta-analysis, Biomed Res Int 2014:247693, 2014. Baillie J: Sphincter of Oddi dysfunction, Curr Gastroenterol Rep 12: 130�134, 2010. Bang S, et al: the medical usefulness of 18-fluorodeoxyglucose positron emission tomography in the differential analysis, staging, and response analysis after concurrent chemoradiotherapy for pancreatic most cancers, J Clin Gastroenterol 40:923�929, 2006. Bar-Meir S, et al: Frequency of papillary dysfunction amongst cholecystectomized patients, Hepatology four:328�330, 1984. Boulahdour H, et al: the hot spot hepatobiliary scan in focal nodular hyperplasia, J Nucl Med 34:2105�2110, 1993. Brunot B, et al: Biopsy and quantitative hepatobiliary scintigraphy within the evaluation of liver transplantation, J Nucl Med 35:1321�1327, 1994. Cicala M, et al: Quantitative cholescintigraphy within the evaluation of choledochoduodenal bile move, Gastroenterology a hundred:1106�1113, 1991. Cicala M, et al: Outcome of endoscopic sphincterotomy in post cholecystectomy sufferers with sphincter of Oddi dysfunction as predicted by manometry and quantitative choledochoscintigraphy, Gut 50: 665�668, 2002. Davenport M: A problem on the utilization of the words embryonic and perinatal within the context of biliary atresia, Hepatology forty one:403�404, writer reply 404-405, 2005. Dimitroulopoulos D, et al: Long performing octreotide within the remedy of advanced hepatocellular cancer and overexpression of somatostatin receptors: randomized placebo-controlled trial, World J Gastroenterol thirteen:3164�3170, 2007. Eppard E, et al: Ethanol-based post-processing of generator-derived 68 Ga towards kit-type preparation of 68Ga-radiopharmaceuticals, J Nucl Med fifty five:1023�1028, 2014. Esmaili J, et al: Correlation of liver-spleen scan findings with modified Child-Pugh classification, Rev Esp Med Nucl 27:99�102, 2008. Herman P, et al: Hepatic adenoma and focal nodular hyperplasia: differential prognosis and treatment, World J Surg 24:372�376, 2000. Kaemmerer D, et al: Neoadjuvant peptide receptor radionuclide therapy for an inoperable neuroendocrine pancreatic tumor, World J Gastroenterol 15:5867�5870, 2009. Kaltsas G, et al: Recent advances in radiological and radionuclide imaging and therapy of neuroendocrine tumours, Eur J Endocrinol 151:15�27, 2004. Kennedy A, et al: Radioembolization for the remedy of liver tumors: common rules, Am J Clin Oncol 35:91�99, 2012. Kwatra N, et al: Phenobarbital-enhanced hepatobiliary scintigraphy within the prognosis of biliary atresia: two decades of experience at a tertiary middle, Pediatr Radiol forty three:1365�1375, 2013. Lawrence B, et al: the epidemiology of gastroenteropancreatic neuroendocrine tumors, Endocrinol Metab Clin North Am 40:1�18, vii, 2011. Macaron C, et al: Recurrent stomach pain after laparoscopic cholecystectomy, Cleve Clin J Med seventy eight:171�178, 2011. In Gottschalk A, et al, editors: Diagnostic nuclear medication, Baltimore, 1988, Williams & Wilkins, pp 538�565. Rufini V, et al: Imaging of neuroendocrine tumors, Semin Nucl Med 36:228�247, 2006. Santhosh S, et al: Role of (18)F-fluorodeoxyglucose positron emission tomography/computed tomography in the characterization of pancreatic lots: experience from tropics, J Gastroenterol Hepatol 28:255�261, 2013. Schoder H, et al: 2-[18F]Fluoro-2-deoxyglucose positron emission tomography for the detection of illness in sufferers with prostatespecific antigen relapse after radical prostatectomy, Clin Cancer Res eleven:4761�4769, 2005. Shamsi K, et al: Focal nodular hyperplasia of the liver: radiologic findings, Abdom Imaging 18:32�38, 1993. Shiomi S, et al: Usefulness of positron emission tomography with fluorine-18-fluorodeoxyglucose for predicting consequence in sufferers with hepatocellular carcinoma, Am J Gastroenterol 96:1877�1880, 2001. Sostre S, et al: A noninvasive take a look at of sphincter of Oddi dysfunction in postcholecystectomy patients: the scintigraphic score, J Nucl Med 33:1216�1222, 1992. Van Essen M, et al: Peptide receptor radionuclide therapy with 177 Lu-octreotate in sufferers with foregut carcinoid tumours of bronchial, gastric and thymic origin, Eur J Nucl Med Mol Imaging 34: 1219�1227, 2007. Van Essen M, et al: Report on short-term unwanted effects of treatments with 177Lu-octreotate in combination with capecitabine in seven sufferers with gastroenteropancreatic neuroendocrine tumours, Eur J Nucl Med Mol Imaging 35:743�748, 2008. Waldherr C, et al: Tumor response and scientific benefit in neuroendocrine tumors after 7. Wang X, et al: Comprehensive analysis of a somatostatin-based radiolabelled antagonist for diagnostic imaging and radionuclide remedy, Eur J Nucl Med Mol Imaging 39:1876�1885, 2012. Wild D, et al: First clinical evidence that imaging with somatostatin receptor antagonists is feasible, J Nucl Med 52:1412�1417, 2011. Wild D, et al: Comparison of somatostatin receptor agonist and antagonist for peptide receptor radionuclide remedy: a pilot examine, J Nucl Med 55:1248�1252, 2014. Williams W, et al: Scintigraphic variations of regular biliary physiology, J Nucl Med 25:160�165, 1984. Helical scanning makes use of a slip ring to enable steady tube gantry rotation while the affected person moves easily by way of the bore, rising scanning speed. Increasing the variety of skinny z-axis detector rows captured extra of the X-rays emitted by the tube cathode (effectively acquiring several axial slices at a time) allowing even sooner scanning and much smaller slice thickness (z-axis resolution). The discount in scanning instances of even massive body segments to a number of seconds, nicely under the edge for a typical breathhold, greatly decreased movement artifacts and allowed multiphasic evaluation (hepatic arterial, portal venous, and delayed phases) of the liver and pancreas. More than one acquisition via the liver is now attainable in a single breathhold. Thinner collimation improves decision and will increase detection of small hepatic lesions by as a lot as 46% (Weg et al, 1998). At present array sizes (most trendy scanners now use no less than sixty four to 128 detector rows), resolution substantially beneath 1 mm is now obtainable in all planes. Scan resolution equal in all planes-perfect cubes of imaging data or "voxel isotropy" (which was achieved by the generation of 16-detector scanners in 2002)-yields smoother photographs when the info acquired in the axial aircraft are reformatted in the coronal, sagittal, and indirect planes. Scrolling quickly through overlaid adjoining picture slices ("cine" viewing) aids appreciation and analysis of tubular and different constructions whose course is skewed to the axial aircraft, similar to dilated bile ducts and hepatic vessels. The capability to enlarge photographs and alter their distinction and brightness on the fly also greatly facilitates picture interpretation. A major downside stays usage of ionizing radiation, with a trend in previous many years towards growing exposure of the patient inhabitants to nontrivial doses, a problem attracting increasing in style scrutiny and spurring substantial ongoing consideration among technical innovators. The right hepatic artery (long open arrow)andthelefthepaticartery(small open arrow)originatefromthe properhepaticartery. Three-dimensional reformatted picture reveals the course of the left portal vein, which ascends in the umbilical fissure earlier than looping anteriorly and inferiorly (short arrow) to department into the medial(arrowhead)andlateral(long arrow)sectoralbranches. With more powerful pc hardware at present available, newer, beforehand prohibitively processorintensive iterative reconstruction algorithms are now approaching scientific availability. For the liver, biliary system, and pancreas, purposes include "materialspecific imaging" and "digital monochromatic imaging" (Morgan, 2014). In the liver, "digital iron images" could also be used for quantitation of hepatic iron deposition without interference from coexisting steatosis (Joe et al, 2012), whereas "virtual non-iron photographs" may be created for fats quantitation independent of concomitant siderosis (Zheng et al, 2013). Lower-energy virtual monochromatic images can also provide more strong surface-rendered 3D arterial images, whereas digital higherenergy pictures have less obvious metallic artifact round biliary stents and clips (Morgan, 2014).
Cheap clarinex 5 mg amex
Following normal cholecystectomy allergy treatment essential oils cheap clarinex 5 mg with amex, a portion of the frequent duct is isolated for choledochoenteric anastomosis allergy shots in pregnancy buy generic clarinex 5mg on-line. A 60- to 70-cm segment of bowel is used for the Roux-en-Y limb allergy symptoms adults trusted 5mg clarinex, and a side-to-side choledochojejunostomy is then constructed 10 to 15 cm from the tip of the jejunal limb. The blind limb of the jejunal access loop is then brought via the fascia of the stomach wall in the right upper quadrant at a point that will permit quick access to the biliary tree. The availability of the cutaneous stoma significantly facilitates subsequent remedy of the residual stones and strictures. After completion of radiologic remedy, the stoma is mobilized, closed, and left buried in the subcutaneous tissues for future entry (Gott et al, 1996). At the identical time, the bypass supplies effective preliminary biliary drainage of the biliary tree and alleviates any immediate biliary sepsis. Clearance of residual stones and dilation of strictures is definitely achieved on an outpatient foundation. The therapy of recurrent stones or strictures is significantly simplified by access to the cutaneous jejunal limb, and it avoids the need for high-risk reoperative biliary procedures (Gott et al, 1996). Patient outcome (death) was subsequently correlated with a variety of collected variables through multivariable logistic regression. The presence of opportunistic infections and an elevated alkaline phosphatase degree (>1000 U/L) had been adverse prognostic indicators of survival. A multidisciplinary method to this dysfunction is important, particularly as a result of the illness rapidly changes, depending on therapy. Survival rates have been low, with 1- and 2-year survival as little as 14% to 41% and 8%, respectively, with a mean reported survival of seven to 12 months (Bouche et al, 1993; Cello & Chan, 1995). For survivors, an association with subsequent cholangiocarcinoma has additionally been reported (Hocqueloux & Gervais, 2000). Immunoglobulin G4�Associated Cholangitis Although the systemic ailments related to immunoglobulin G4 (IgG4) have been acknowledged since the 1960s (Sarles et al, 1961), the credit score for the first description IgG4 cholangitis belongs to Montefusco and colleagues (1984), who described a series of case stories of patients with mixed pancreatic and extrapancreatic disease related to elevated IgG4. In the biggest reported cohort to date, which includes fifty three patients, Ghazale and colleagues (2008) described probably the most frequent scientific signs and symptoms at presentation of IgG4 cholangitis: jaundice (77%), weight loss (51%), mild to moderate belly ache (26%), steatorrhea (15%), and new-onset diabetes (8%). The diagnostic criteria for IgG4 cholangitis are either having a earlier analysis of IgG4-related pancreatic/ biliary illness or two or more of the next: elevated serum IgG4, other manifestation of a systemic illness, or bile duct biopsy exhibiting greater than 10 IgG4-positive cells per highpower field with a documented response after four weeks of steroid remedy (Ghazale et al, 2008). Liver histology in IgG4associated cholangitis is characterised by lymphoplasmacytic infiltrates within and round bile ducts and obliterative phlebitis and fibrosis resulting in sclerosis of the bile ducts. A persistent two or threefold elevation of the alkaline phosphatase stage is typical (Gordon, 2008). The radiologic inclusion criteria embody the presence of diffusely distributed strictures of the biliary system seen on cholangiography and attribute hepatic histology. The histology, categorized by Ludwig and colleagues (1981), contains 4 stages: (1) periportal hepatitis, (2) periportal hepatitis and fibrosis, (3) fibrosis extending beyond the limiting plate, and (4) biliary cirrhosis. Accurate analysis is of utmost importance to stop unnecessary surgery and avoid delayed analysis of a doubtlessly deadly malignancy. In common, these abscesses ought to be handled following commonplace surgical principles of drainage and broad-spectrum antibiotics, until the fever resolves and liver function exams return to normal (Rintoul et al, 1996) (see Chapter 72). Traditionally, remedy consists of antibiotic administration and drainage of purulent collections. Although this remains the standard strategy to the affected person with hepatic abscess, some investigators have advocated using antibiotics alone in chosen patients (Pearce et al, 2003). Over the previous decade, percutaneous aspiration of pyogenic liver abscess with out catheter drainage has additionally gained elevated consideration. Retrospective sequence have reported percutaneous aspiration success rate in combination with antibiotic remedy to be within the vary of 58% to 88%, which is similar to the outcomes of catheter drainage (Barakate et al, 1999; Johannsen et al, 2000; Seeto & Rockey, 1996). However, you will want to mention that no randomized trial comparing percutaneous aspiration and catheter drainage of liver abscesses has been performed. Antibiotics should be began as soon as attainable, as quickly as the prognosis of pyogenic liver abscess is suspected. Blood specimens for culture must be obtained before initiating empiric remedy, but delaying therapy until abscess materials is obtained is potentially dangerous and ill advised. Pyogenic liver abscesses that come up in a affected person with biliary illness typically include enterococci and enteric gram-negative bacilli. Pyogenic liver abscesses from a colonic or pelvic source are more commonly the outcomes of coliforms and anaerobes. Metronidazole should be included within the initial remedy for most cases of pyogenic liver abscess to empirically treat essentially the most commonly discovered anaerobes, particularly Bacteroides fragilis and Entamoeba histolytica, whereas the particular etiology is being evaluated. Once microbiologic information are obtained, antibiotic therapy must be tailor-made to the organisms isolated and their respective antibiotic susceptibility profiles. Other anaerobes less generally discovered are: Fusobacterium, Clostridium, anaerobic Streptococci and Streptococcus milleri (Johannsen et al, 2000). Pyogenic liver abscesses are normally handled initially with parenteral antibiotic remedy for two to 3 weeks, and patients subsequently full a 4- to 6-week course of oral antibiotics (Pitt, 1990). On event, a residual cavity persists regardless of extended therapy; if the dimensions of this cavity is stable on serial imaging research and the affected person is asymptomatic, antibiotics may be stopped and the affected person observed carefully for the event of recurrent fevers or abdominal pain. In the setting of acute cholangitis, intervention ought to start with resuscitation, parenteral antibiotics, and biliary decompression. The imaging and procedural modalities used in the remedy of affected patients require a thorough understanding of the etiology and should be tailored to the particular causation. Badaro R, et al; the Latin American Antibiotic Research Group: A multicenter comparative research of cefepime versus broad-spectrum antibacterial therapy in reasonable and severe bacterial infections, Braz J Infect Dis 6:206�218, 2002. Bile Duct Lithotripsy Prospective Study, Ann Surg 209:743�753, dialogue 753-735, 1989. Boender J, et al: Endoscopic sphincterotomy and biliary drainage in patients with cholangitis as a end result of common bile duct stones, Am J Gastroenterol 90:233�238, 1995. Chen C, et al: Reappraisal of percutaneous transhepatic cholangioscopic lithotomy for primary hepatolithiasis, Surg Endosc 19:505� 509, 2005. Csendes A, et al: Bacteriological studies of liver parenchyma in controls and in sufferers with gallstones or widespread bile duct stones with or without acute cholangitis, Hepatogastroenterology forty two:821�826, 1995. Csendes A, et al: Counts of micro organism and pyocites of choledochal bile in controls and in patients with gallstones or widespread bile duct stones with or with out acute cholangitis, Hepatogastroenterology forty three: 800�806, 1996. Ducreux M, et al: Management of malignant hilar biliary obstruction by endoscopy: outcomes and prognostic elements, Dig Dis Sci 37:778� 783, 1992. Ghazale A, et al: Immunoglobulin G4-associated cholangitis: medical profile and response to remedy, Gastroenterology 134:706� 715, 2008. Harz C, et al: Extracorporeal shock-wave lithotripsy and endoscopy: combined therapy for problematic bile duct stones, Surg Endosc 5:196�199, 1991. In Root R, Trunkey D, et al, editors: New surgical and medical approaches in infectious diseases, New York, 1987, Churchill Livingstone, pp 113�132. Kadir S, et al: Percutaneous biliary drainage within the management of biliary sepsis, Am J Roentgenol 138:25�29, 1982.
Generic clarinex 5 mg on line
Vera A allergy shots guidelines order clarinex 5mg mastercard, et al: Risk factors for recurrence of main sclerosing cholangitis of liver allograft allergy testing orlando buy clarinex 5mg on line, Lancet 360:1943�1944 allergy forecast reston va purchase 5 mg clarinex, 2002. Wagner S, et al: Endoscopic management of biliary tract strictures in primary sclerosing cholangitis, Endoscopy 28:546�551, 1996. Wilschanski M, et al: Primary sclerosing cholangitis in 32 youngsters: scientific, laboratory, and radiographic features, with survival analysis, Hepatology 22:1415�1422, 1995. Yamada S, et al: Small duct cholangitis induced by N-formyl L-methionine L-leucine L-tyrosine in rats, J Gastroenterol 29:631�636, 1994. By definition, a biliary fistula is an abnormal communication between the biliary tract and different organs. In distinction, a biliary stricture is defined as an irregular narrowing of the bile duct that will result in obstruction and fistula. Internal biliary fistulae are uncommon and usually spontaneous and without a significant assortment of bile. A controlled fistula has no related vital assortment of bile; an uncontrolled fistula denotes a communication with an inner assortment of bile. The terms benign biliary stricture and fistula are often used interchangeably when referring to external biliary fistula and iatrogenic injuries. In distinction to malignant biliary obstruction, by which short-term palliation is commonly the goal of therapy, benign strictures require sturdy restore as a result of most patients are anticipated to live for many years. Regardless of the nature of the biliary fistulae and strictures, management of sufferers with this condition is optimized when therapy is directed by a extremely specialized multidisciplinary staff composed of experienced interventional radiologists, diagnostic radiologists, gastroenterologists, and surgeons. Center during the years 1932 via 1978, the incidence of biliary-enteric fistula was zero. A giant series from Greece (Lygidakis, 1981) confirmed an incidence of 2%, and in Native Americans, the incidence is 3. In Japan, the place bilirubin stones and first intraductal disease predominate, the incidence of fistula is between 0. The kind of fistula famous on this group of sufferers normally entails the ductal system somewhat than the gallbladder. The pathogenic sequence of events for calculous biliary tract disease has been nicely described by Glenn and Mannix (1957). It consists of pressure necrosis and erosion of a part of the biliary tract wall into an adjacent construction to which it has become adherent in the midst of repeated bouts of inflammation, often with distal biliary tract obstruction. The probability of the branches of the hepatobiliary tree to turn into infected and anatomic proximity to adjoining hollow viscera largely determine the relative incidence of the different types of spontaneous biliary-enteric fistulae secondary to calculous disease. Indeed, repeated attacks of cholecystitis might lead to progressive fibrosis and shrinking of the gallbladder, which in the end obliterates the triangle of Calot. The inflammatory process might unfold to involve the widespread hepatic duct, causing inflammatory stenosis or stricture leading to jaundice and cholangitis. Patients with inflammatory strictures of the extrahepatic bile duct in association with continual cholelithiasis could have radiologic features which may be indistinguishable from cholangiocarcinoma (see Chapter 51) (Hadjis et al, 1985; Standfield et al, 1989; Wetter et al, 1991). Estimates of incidence are crude, gleaned solely from many small collection, normally with fewer than 50 patients. If all types of internal biliary fistula are included, calculous biliary tract illness accounts for 90%; peptic ulcer disease, 6%; and neoplasm, trauma, parasitic an infection, and congenital anomalies make up the remaining 4% (Piedad & Wels, 1972). Overall, 1% to 3% of sufferers with cholethiasis in Western international locations develop biliary-enteric fistula, with a female/male ratio of 3: 1. In 11,808 circumstances of nonmalignant biliary tract illness encountered at New York Hospital/Cornell Medical Fistulae Involving the Gallbladder In Western countries, the place cholesterol cholelithiasis abounds, the gallbladder is most frequently the location of severe inflammation and obstruction (see Chapter 33). Cholecystenteric fistulae represent 70% to 85% of all biliary fistulae reported in the world literature as much as 1982 (Rau et al, 1980; Safaie-Shirazi et al, 1973). Of the 23 instances reported as much as 1978, 21 have been secondary to gallstone illness, and 1 case of each was because of duodenal ulcer and a main carcinoma of the gallbladder (Morris et al, 1978). Modern series of bowel obstructions report gallstone ileus to be a very uncommon trigger (well under 1%). Although most fistulae between the gallbladder and intestinal tract turn out to be apparent preoperatively or intraoperatively, cholecystocholedochal fistulae are insidious and may not be appreciated even at surgery. In both occasion, the mechanism of formation is similar: stress necrosis into the widespread duct by a large solitary impacted calculus. Awareness of this situation is essential and may assist avoid injury to the common duct at operation. This trigger is now a lot much less frequent on account of efficient medical therapy with antacid medicine. Other, much less common causes of choledochoduodenal fistula embody cholelithiasis (see Chapter 32), operative trauma, duodenal diverticula, echinococcal an infection (see Chapter 74), B. The incidence of distal choledochoduodenal fistula secondary to cholelithiasis or operative trauma is variable in several parts of the world. Large sequence from Argentina reported the incidence of distal choledochoduodenal fistula to be zero. Additionally, there are 2 case stories of choledochoduodenal fistula occurring after blunt abdominal trauma (Chao et al, 2008; Tan et al, 2011). This examine additionally discovered an intriguing affiliation between peripapillary fistula with widespread duct stones and complications of cholangitis. Spontaneous fistula formation between the widespread duct and the colon has been recorded only 5 occasions in the English literature (Bannister et al, 1984; Bose & Sastry, 1983; Guitron-Cantu et al, 2001; Rawas et al, 1987). We are also aware of one case of a choledochocolonic fistula that developed after blunt abdominal trauma (Benson et al, 2001) (see Chapter 122) and one other that developed as a complication from diverticulitis (BlancoBenavides & Rodriguez-Jerkov, 1992). Peptic ulcer disease has rarely produced fistulae between the common duct, duodenum, and pancreas (Aitken et al, 1986). More just lately, a bile duct stricture associated with a choledochocolonic fistula was reported following an uncomplicated open cholecystectomy 4 months prior (Munene et al, 2006). Fistulae Involving the Intrahepatic Ducts, Liver, and Lung Thoracobiliary and bronchobiliary fistulae are rare (Boyd, 1977; Chan et al, 1984; Cleve & Correa, 1958) and discuss with communications between the biliary tree and the pleural cavity or bronchial tree. The three major classes of bronchobiliary fistula are these resulting from (1) an infection, (2) trauma, and (3) congenital causes (Liao, 2011; Sane, 1971). Worldwide, the principal explanation for bronchobiliary fistula in adults is parasitic illness of the liver, either echinococcal (see Chapter 74) or amebic (see Chapters forty five and 73). In developed international locations, iatrogenic damage to the biliary system is the most frequent trigger. The hallmark symptom of a bronchobiliary fistula is biliptysis along side other pulmonary complaints, jaundice, cholangitis, and exterior biliary fistula or subphrenic abscess. In the presence of an external fistula, injection of contrast resolution is essentially the most facile and direct strategy. Bronchobiliary fistulae even have been proven by cholescintigraphy (Annovazzi et al, 2008; Andalkar et al, 2004; Gunlemez et al, 2009; Santra et al, 2009; Savitch et al, 1983; Uramoto et al, 2008; Velchik et al, 1991). The surgical treatment of parasitic diseases of the liver is mentioned elsewhere in this guide (see Chapters 45, 73, and 74). In giant collection of surgically treated instances of hepatic echinococcal illness in Greece and Turkey, only 2% had been complicated by rupture into the lung or bronchi (Alestig et al, 1972). Amebic abscess of the liver has been reported in affiliation with bronchobiliary fistula in 8% of instances (Razemon et al, 1963).
Diseases
- Tay syndrome ichthyosis
- Diffuse leiomyomatosis with Alport syndrome
- Deafness nephritis ano rectal malformation
- Ausems Wittebol Post Hennekam syndrome
- Chondroma (benign)
- Elephantiasis
- Lymphocytic infiltrate of Jessner
- Pyelonephritis
Cheap 5 mg clarinex amex
The overriding consideration in sufferers presenting with gallstone obstruction of the intestine ought to be reduction of the life-threatening cause of obstruction allergy under armpits generic clarinex 5mg without prescription. The use of nasogastric decompression and preoperative antibiotics is recommended to decrease the dangers of aspiration and postoperative wound infection allergy kansas city order 5 mg clarinex. Unless the obstructed section is ischemic or has perforated and requires a small bowel resection allergy treatment under tongue clarinex 5mg free shipping, the obstructing calculus can be manipulated proximally to a wholesome part of bowel, the place a protected enterotomy and stone removal may be executed. Jejunal impaction, typically by stones bigger than 4 cm, happens approximately 15% of the time, and enterotomy could additionally be made on the site or simply proximal to it. Duodenal obstruction, usually within the bulb, is named Bouveret syndrome (Argyropoulos et al, 1979; Bhama et al, 2002; Cooper & Kucharski, 1978; Frattaroli et al, 1997; Koulaouzidis & Moschos 2007; Maglinte et al, 1987; Thomas et al, 1976), which happens in 10% of patients and could additionally be dealt with by duodenostomy or pyloroplasty. It often could additionally be potential to manipulate the stone again into the stomach and take away it through gastrotomy. Rarely, a gastroenterostomy is critical to protect a duodenotomy or severely traumatized duodenum at the site of impaction. However, the review of 128 instances by Cappell and Davis (2006) famous marginal success with endoscopy. We are conscious of one case report of a failed endoscopic extraction that led to spontaneous uneventful passage of the stone. In rare situations, the sigmoid colon is the location of obstruction of a calculus that has managed to pass by way of the terminal ileum or enter the colon by way of a cholecystocolic fistula (Anseline, 1981; Clavien et al, 1990). Almost invariably, another pathologic process, corresponding to diverticulitis, has produced an space of colonic narrowing. However, recent stories have described successful administration with enterolithotomy and resection of the fistulous phase (Gupta et al, 2007). Open exploration and enterolithotomy has been the standard surgical method for the therapy of traditional gallstone ileus. These calculi could also be poised for passage via the fistula, presumably to induce a recurrent episode of gallstone ileus, a phenomenon estimated to happen in 5% of cases (Clavien et al, 1990; Haq et al, 1981; Levin & Shapiro, 1980). Recently, extra authors have described laparoscopic or laparoscopic-assisted therapy for patients with gallstone ileus (Allen et al, 2003; Malvaux et al, 2002; Moberg & Montgomery, 2007; Owera et al, 2008; Sesti et al, 2013; Shiwani & Ullah, 2010; Yu et al, 2013; Zygomalas et al, 2012). Yu and colleagues (2013) just lately reported on 34 cases of gallstone ileus handled laparoscopically with satisfactory outcomes. Although the worldwide expertise with laparoscopic management of gallstone ileus is growing, the existing literature is based completely on small numbers of sufferers and case reports. Because of those limitations, the efficacy and security of this strategy remains unclear, though the out there reports recommend favorable outcomes in chosen sufferers. There is considerable debate within the surgical literature as to whether or not cholecystectomy, frequent duct exploration, and/or dismantling and closure of the cholecystenteric fistula should accompany enterotomy and relief of the obstruction or await a second operation (Kirchmayr et al, 2005; Muthukumarasamy et al, 2008; Zuegel et al, 1997). Historical data of revealed reports from the years 1953 via 1993 (Reisner & Cohen, 1994) confirmed a lower mortality price of eleven. Several published reports indicated that operative mortality is decrease in these critically unwell, aged sufferers when only the gallstone obstruction is relieved (Heuman et al, 1980; Kasahara et al, 1980; Muthukumarasamy et al, 2008; Tan et al, 2004; VanLandingham & Broders, 1982). This has led to the final agreement that enterolithotomy alone must be accomplished for fragile sufferers with important comorbidities and that the single-stage process ought to be reserved for young, match, and low-risk patients. The authors evaluated 127 cases of gallstone ileus and famous a 6% 30-day mortality and 35% morbidity rate; 14 patients underwent cholecystectomy at the time of index operation. Interestingly, there was no vital difference between the 2 cohorts with regard to age, comorbid situations, preoperative sepsis, classification as an emergent process, or differences in morbidity or mortality charges. Taken together, this report suggests that cholecystectomy and enterolithotomy may be safer than traditionally reported (Mallipeddi et al, 2013; Yu et al, 2013). We recommend sustaining a conservative approach in such sufferers and would solely think about cholecystectomy within the clinically secure patient. Indeed, careful follow-up of sufferers treated with enterolithotomy alone signifies that one third to one half may have minimal or no signs after reduction of the gallstone ileus, and no additional treatment shall be needed (Clavien et al, 1990; Tan et al, 2004; van Hillo et al, 1987). It is important to do not overlook that recurrence of gallstone ileus in patients handled with enterolithotomy alone is estimated to be between 5% and 10% (Lassandro et al, 2005; Mallipeddi et al, 2013). As talked about, operative mortality rates were reported at 15% to 25% in large reported series till the early Nineteen Seventies. Reductions in operative mortality charges have been attainable by limiting treatment to enterotomy and stone removing alone with out additional surgical therapy in high-risk patients (Ayantunde & Agarwal, 2007; Glenn et al, 1981; Mallipeddi et al, 2013; Muthukumarasamy et al, 2008; Rodriguez-Sanjuan et al, 1997; Tan et al, 2004). If an asymptomatic or mildly symptomatic cholecystenteric fistula is diagnosed preoperatively, lots of the management decisions relating to gallstone ileus discussed previously may apply. Elective surgery might by no means be necessary in a totally asymptomatic individual, and surgery could present an unfavorable risk-to-benefit ratio in an aged, minimally symptomatic patient. Along with dismantling of the fistula and administration of widespread duct stones, different options to cholecystectomy should be considered, such as a interval of expectant administration with cautious observation, endoscopic papillotomy and stone extraction with the gallbladder left in situ, or interval cholecystectomy if signs of ache or cholangitis persist after endoscopic biliary surgery. In a relatively healthy patient, we consider that cholecystectomy, closure of the fistula, and therapy of any widespread duct pathology promise the best longterm therapeutic result (Chikamori et al, 2001; Crouch & Kuhnke, 2000; Kwon & Inui, 2007; Lee et al, 2004; Rohatgi & Singh, 2006; Wang et al, 2006). One operative consideration is to perform a cholecystostomy and extraction of huge calculi, which should add little further threat. If one is going to proceed with definitive cholecystectomy and closure of the fistula, consideration should be given to performing an operative cholangiogram to rule out frequent duct stones. Cholecystocolic Fistulae and Choleric Enteropathy A cholecystocolic fistula could develop acutely in sufferers with long-standing gentle or reasonably symptomatic biliary tract illness and may be heralded by a sudden change in bowel habits with a number of, unfastened stools and the event of fever, chills, and different signs of cholangitis from colonic bacterial reflux into the biliary tract. There is a female predominance with approximately a 3:1 ratio (Costi et al, 2009). Increased stool frequency persists, particularly after ingestion of food, and bouts of fever and malaise subside. Other characteristic symptoms then seem, similar to eructation, nausea, weight loss, and growing diarrhea and steatorrhea. These latter signs precede the onset of choleric enteropathy, a dramatic complication of cholecystocolonic fistula. This enteropathy is also seen in other main disturbances of bile acid metabolism, such as with main ileal resection or blind loop syndrome (Brandt, 1984). Choleric enteropathy includes a wide spectrum of anatomic, physiologic, and biochemical modifications produced by a significant alteration of the enterohepatic circulation. The malabsorption syndrome secondary to cholecystocolonic fistula was clinically documented first by Augur and Gracie (1970) and has since been studied by others (Rau et al, 1980). Ordinarily, 95% of bile acids are handed down the jejunum, aiding in fats and cholesterol absorption, earlier than being largely reabsorbed within the terminal ileum as part of an efficient enterohepatic circulation. Two or three cycles of the bile acid pool per meal occur, with further metabolism of bile acids within the colon and very little misplaced. With a cholecystocolic fistula, however, a large a half of the entire major bile acid pool is lost directly into the colon, resulting in a excessive luminal concentration of bile acids. In the colon, the primary bile acids undergo deconjugation and dehydroxylation by fecal bacteria, and this elevated concentration of bile acids induces a water secretory diarrhea. Depending on the quantity of bile still passing through the frequent duct into the small bowel, fat absorption is affected, which over time may result in fatty-acid diarrhea. More instantly, nevertheless, colonic secretion of water and electrolytes is maximally stimulated by bile acids.
Buy clarinex 5mg overnight delivery
Readmission for gallstone related problems (pancreatitis allergy testing sarasota purchase 5mg clarinex fast delivery, cholecystitis allergy shots didn't work discount 5mg clarinex with amex, cholangitis allergy forecast in dallas purchase clarinex 5 mg on-line, jaundice, colic) have been considerably extra frequent within the interval group than the same-admission group (17% vs. These results remained vital when comparing patients with endoscopic sphincterotomy in a subgroup analysis. As with the previous retrospective studies, there was no distinction in size of stay, A. Gallstones and Gallbladder Chapter 36C Stones in the bile duct: endoscopic and percutaneous approaches 621 issue of surgical procedure, conversions from laparoscopic to open surgery, or well being care use between the 2 groups. Usually a delay in surgery in these patients is secondary to critical sickness or while awaiting other surgical or endoscopic treatments for problems corresponding to a cyst-gastrostomy for a pseudocyst or debridement of walled-off pancreatic necrosis. In the acute setting, an endoscopic strategy to biliary pancreatitis offers the theoretical benefit of quick aid of ampullary obstruction and ductal clearance without the risks of surgery. Patients with gentle pancreatitis had similar outcomes no matter remedy strategy. Overall, no vital differences had been discovered within the incidences of either native (10. Patients with biliary obstruction and cholangitis were also included on this study. The remaining 205 patients were randomized to standard treatment or sphincterotomy regardless of the cholangiographic findings. Compared with conventional therapy, the authors showed a significant advantage for sufferers handled endoscopically with respect to morbidity (17% vs. The total mortality and complication charges had been similar between the 2 groups whatever the severity of pancreatitis, but the price of serious respiratory failure was higher in the invasive group (P =. A latest metaanalysis of the seven identified well-designed, randomized, controlled trials on this topic confirms these similar findings (Uy et al, 2009). Endoscopic strategies are nicely established, and accessories have been developed to improve success and safety. Advancement in endoscopic techniques allows the administration of complicated bile duct stone disease. Patients with acute cholangitis ought to be thought of for pressing endoscopic administration. Integrated endoscopic remedy for biliary illness is nicely established in facilities where surgeons and endoscopists work carefully collectively and provide one another with an appropriate discussion board for important analysis of different therapeutic techniques. Gallstones and Gallbladder Chapter 36C Stones within the bile duct: endoscopic and percutaneous approaches 622. Das A, et al: Treatment of biliary calculi utilizing holmium:yttrium aluminium garnet laser, Gastrointest Endosc forty eight:207�209, 1998. Deviere J, et al: Successful management of benign biliary strictures with absolutely lined self-expanding metallic stents, Gastroenterology 147:385� 395, 2014. Diaz D, et al: Methyl tert-butyl ether within the endoscopic remedy of widespread bile duct radiolucent stones in elderly sufferers with nasobiliary tube, Dig Dis Sci 37:97�100, 1992. DiSario J, et al: Biliary and pancreatic lithotripsy units, Gastrointest Endosc sixty five:750�756, 2007. Ersoz G, et al: Biliary sphincterotomy plus dilation with a large balloon for bile duct stones which are troublesome to extract, Gastrointest Endosc fifty seven:156�159, 2003. Escourrou J, et al: Early and late complications after endoscopic sphincterotomy for biliary lithiasis, with and with out the gallbladder "in situ. The German Study Group on Acute Biliary Pancreatitis, N Engl J Med 336:237�242, 1997. Garcia-Cano J, et al: Fully coated self-expanding metal stents within the administration of adverse widespread bile duct stones, Rev Esp Enferm Dig a hundred and five:7�12, 2013. Akcakaya A, et al: Mechanical lithotripsy and/or stenting in administration of difficult widespread bile duct stones, Hepatobiliary Pancreat Dis Int eight:524�528, 2009. Arya N, et al: Electrohydraulic lithotripsy in 111 sufferers: a secure and efficient remedy for troublesome bile duct stones, Am J Gastroenterol ninety nine:2330�2334, 2004. Bhandari S, et al: Usefulness of single-operator cholangioscope-guided laser lithotripsy in sufferers with Mirizzi syndrome and cystic duct stones: experience at a tertiary care center, Gastrointest Endosc 2016; Jan 5 [Epub forward of print]. Boerma D, et al: Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile duct stones: a randomized trial, Lancet 360:761�765, 2002. Burdick J, et al: Holmium laser for therapy of left hepatic duct stone, Gastrointest Endosc 48:523�526, 1998. Cerefice M, et al: Complex biliary stones: therapy with elimination selfexpandable metallic stents: a new method (with videos), Gastrointest Endosc 74:520�526, 2011. Classen M, Demling L: Endoscopische Sphinkterotomie der Papilla Vater, Dtsch Med Wochenschr ninety nine:496�497, 1974. Grimm H, Soehendra N: Unterspritzung zur Behandlung der Papillotomie-Blutung, Dtsch Med Wochenschr 108:1512�1514, 1983. Hirano T, et al: A potential mechanism for gallstone pancreatitis: repeated short-term pancreaticobiliary duct obstruction with exocrine stimulation in rats, Proc Soc Exp Biol Med 202:246�252, 1993. Hochberger J, et al: Management of adverse widespread bile duct stones, Gastrointest Endosc Clin N Am 13:623�634, 2003. Ikeda S, et al: Endoscopic sphincterotomy: long-term ends in 408 patients with full follow-up, Endoscopy 20:13�17, 1988. Inamdar S, et al: Pregnancy is a risk factor for pancreatitis after endoscopic retrograde cholangiopancreatography in a nationwide cohort study, Clin Gastroenterol Hepatol 14:107�114, 2016. Iwashita T, et al: Endoscopic ultrasound-guided rendezvous for biliary access after failed cannulation, Endoscopy 44:60�65, 2012. Katsinelos P, et al: the effect of indwelling endoprosthesis on stone size or fragmentation after long-term treatment with biliary stenting for giant stones, Surg Endosc 17:1552�1555, 2003. Kawai K, et al: Endoscopic sphincterotomy of the ampulla of Vater, Gastrointest Endosc 20:148�151, 1974. Kiil J, et al: Large bile duct stones treated by endoscopic biliary drainage, Surgery a hundred and five:51�56, 1989. Kim U, Bosner B: Timing of surgery for acute gallstone pancreatitis, Am J Surg 156:393�396, 1988. Leese T, et al: Successes, failures, early issues and their management following endoscopic sphincterotomy: leads to 394 consecutive patients from a single centre, Br J Surg seventy two:215�219, 1985. Madhoun M, et al: Endoscopic papillary giant balloon dilation reduces the necessity for mechanical lithotripsy in sufferers with massive bile duct stones: a scientific evaluate and meta-analysis, Diagn Ther Endosc 2014:309618, 2014. Mador B, et al: Early versus delayed cholecystectomy following endoscopic sphincterotomy for mild biliary pancreatitis, Surg Endosc 28: 3337�3342, 2014. Maleux G, et al: Embolization of post-biliary sphincterotomy bleeding refractory to medical and endoscopy therapy: technical outcomes, medical efficacy and predictors of end result, Eur Radiol 24:2779�2786, 2014. Mavrogiannis C, et al: Needle-knife fistulotomy versus needle-knife precut papillotomy for the treatment of common bile duct stones, Gastrointest Endosc 50:334�339, 1999. Maydeo A, et al: Single operator cholanioscopy-guided laser lithostripsy in sufferers with difficult biliary and pancreatic ductal stones, Gastrointest Endosc 74:1308�1314, 2011. Murphy P, et al: Implementation of an acute care surgical procedure service facilitates fashionable scientific follow tips for gallstone pancreatitis, J Am Coll Surg 221:975�981, 2015. Nakajima M, et al: Five years experience of endoscopic sphincterotomy in Japan: a collective research from 25 facilities, Endoscopy 2:138�141, 1979.

Order clarinex 5 mg without prescription
Hull D allergy medicine upset stomach trusted clarinex 5 mg, et al: Management of cholelithiasis in heart and lung transplant sufferers: with evaluation of laparoscopic cholecystectomy allergy herbs discount clarinex 5 mg with visa, Conn Med fifty eight:643�647 zopiclone allergy symptoms buy clarinex 5 mg otc, 1994. Jayaraman S, et al: Getting started with robotics normally surgery with cholecystectomy: the Canadian experience, Can J Surg 52(5):374� 378, 2009. Jones D, et al: the influence of intraoperative gallbladder perforation on long-term outcome after laparoscopic cholecystectomy, Surg Endosc 9:977�980, 1995. Kane R, et al: the outcomes of elective laparoscopic and open cholecystectomy, J Am Coll Surg one hundred eighty:136�145, 1995. Mayumi T, et al: Results of the Tokyo Consensus Meeting Tokyo Guidelines, J Hepatobiliary Pancreat Surg 14(1):114�121, 2007. Pesce A, et al: Bile duct harm throughout laparoscopic cholecystectomy without intraoperative cholangiography: a retrospective examine on 1,a hundred selected patients, Dig Surg 29(4):310�314, 2012. Ransohoff D, et al: Prophylactic cholecystectomy or expectant administration for silent gallstones: a call evaluation to assess survival, Ann Intern Med ninety nine:199�204, 1983. Ros A, et al: Laparoscopic cholecystectomy versus mini-laparotomy cholecystectomy: a potential, randomized, single-blind study, Ann Surg 234(6):741�749, 2001. Rosemurgy A, et al: Does the worth of robotic cholecystectomy translate to a monetary burden Soper N, et al: Diagnosis and management of biliary complications of laparoscopic cholecystectomy, Am J Surg a hundred sixty five:663�669, 1993. Steck T, et al: Prevalence and management of cholelithiasis in heart transplant patients, J Heart Lung Transplant 10:1024�1032, 1991. Therefore warning must be used in extrapolating these data to the fashionable endoscopic expertise. This process is enough for most patients, and the overall failure price is has been reported as low as 3% (Girard & Legros, 1981). Others, however, have reported considerably greater failure rates (Allen et al, 1981; Saharia et al, 1977), which has prompted some authors (Allen et al, 1981; Lygidakis, 1982) to recommend biliary-enteric drainage in all patients with earlier choledocholithotomy. In basic, biliary-enteric drainage at reoperation is acceptable within the following scenarios: (1) stricture or stenosis of the distal bile duct or sphincter of Oddi, (2) marked dilation of the duct of two cm or extra, (3) multiple or primary bile duct stones, (4) incapability to remove all stones from the duct, and (5) a 3rd operation. Transduodenal sphincteroplasty, choledochoduodenostomy, and choledochojejunostomy are efficient strategies of biliary enteric drainage (Braasch et al, 1980; Johnson & Harding Rains, 1978; Jones, 1978) (see Chapter 31). Occasionally, recurrent or main stones will be seen in patients with dilated ducts and a widely patent sphincter after sphincteroplasty or sphincterotomy. In such circumstances, choledochoduodenostomy or Roux-en-Y choledochojejunostomy is important. In the context of earlier biliary pancreatitis, sufferers who current for reoperation with a number of stones and an incompletely cleared proximal biliary system could also be better served with an end-to-side choledochoduodenostomy versus a side-to-side method because it minimizes the prospect of stones dropping distally and inflicting recurrent pancreatitis. Sump syndrome is an uncommonly observed complication of choledochoduodenostomy and ought to be managed initially by endoscopic modalities. Clinical Experience With Reoperation Girard (2000) reviewed all patients who underwent reoperation for retained or recurrent choledocholithiasis on the MaisonneuveRosemont Hospital between 1969 and 1990. Eighty-five sufferers with preoperatively confirmed choledocholithiasis underwent a total of 88 operations. Eighty-five of those operations were second procedures, and three sufferers required a third operation. Three types of bile duct reoperation had been performed: choledocholithotomy with T-tube drainage (64 patients), choledocholithotomy with side-to-side choledochoduodenostomy (15 patients), and choledocholithotomy with transduodenal sphincteroplasty (6 patients). Choledocholithotomy with T-tube drainage in 1 affected person and choledocholithotomy with side-to-side choledochoduodenostomy in 2 patients have been performed at a 3rd operation. There were no deaths in the sequence even though 43 of eighty five patients have been older than age 60 years and 44 sufferers had associated threat elements. Stones impacted at the ampulla could be damaged down and eliminated by way of a supraduodenal strategy; nevertheless, a transduodenal sphincteroplasty is usually much less traumatic. Clearance of the biliary tree ought to be confirmed by performing postexploratory choledochoscopy and cholangiography. The worth of choledochoscopy has been confirmed by many authors (Dayton et al, 1984; Kappes et al, 1982; Nora et al, 1977). Postexploratory cholangiography must also be carried out previous to closure of the stomach, not solely as a end result of it could find missed stones, but in addition because it may reveal unsuspected disruption of the biliary ductal system. If cholangiography approach is meticulous, issues with false positives from air bubbles and poor opacification of the entire system may be largely eliminated to provide constant and reliable cholangiograms. The selective use of biliary-enteric drainage procedures is another technique to lower the incidence of subsequently symptomatic retained stones. If these circumstances pertain in an aged or poor-risk patient, choledochoduodenostomy might obviate reexploration. Other indications embrace (1) the presence of irretrievable intrahepatic stones, (2) proven ampullary stenosis, or (3) an impacted ampullary stone. In certainly one of these collection (McSherry & Glenn, 1980), choledocholithotomy was carried out for retained or recurrent stones in 341 patients; 7 sufferers died after the process, leading to a mortality of 2%. If three of these deaths that occurred after pressing operations for cholangitis or pancreatitis are excluded, nonetheless, and only the elective procedures are considered, only 4 patients died (1%) after repeat choledocholithotomy. These results present that the overall mortality rate for retained or recurrent stones is less than 2%, with most deaths occurring in aged patients. Surgery stays a important element of the armamentarium that can be utilized to treat recurrent bile duct stones. Gastroenterologists, radiologists, and surgeons should work together carefully to assess the most acceptable intervention for a person affected person. If unsuccessful or contraindicated, operative administration is an inexpensive different. Surgical intervention has a excessive success rate and acceptable charges of mortality and morbidity. These findings must be confirmed through intraoperative cholangiography and complete clearance of the biliary tree documented with completion cholangiography and choledochoscopy. Supraduodenal Choledochotomy and Exploration of the Common Bile Duct Exposure the liver is retracted superiorly with a broad-bladed, slightly curved retractor, similar to a Hartmann ("sweetheart") retractor. This retractor must be deep sufficient to displace the liver however not so curved as to traumatize it. A pack must be put over the hepatic flexure of the colon right down to the hepatorenal pouch and the medial part of the duodenum. The lesser omentum and stomach are retracted to the left after placement of another pack. Choledochotomy A distal vertical supraduodenal choledochotomy is generally most well-liked for a quantity of causes. First, as a end result of a choledochoduodenostomy may be required (see Chapter 31), the opening A. Second, a distal choledochotomy leaves the maximal quantity of bile duct proximally in order that it may be used in the future for a further procedure. The anatomy of the cystic duct is very variable, and care should be exercised to open the proper duct (see Chapter 2).
Buy 5mg clarinex visa
It is necessary to scan sufferers in several positions to differentiate gallstones from polyps allergy forecast dallas fort worth buy clarinex 5mg amex, because gallstones are cellular allergy urticaria treatment cheap 5 mg clarinex visa, whereas polyps are mounted allergy testing boulder purchase clarinex 5 mg on-line. Technical components that may optimize demonstration of acoustic shadowing from small gallstones include rising transducer frequency, setting the focal zone at depth of the gallstones, positioning the affected person such that multiple stones will cluster collectively, and demonstrating twinkle artifact on color Doppler. Stones in the gallbladder neck could additionally be tough to visualize however ought to roll into the gallbladder body or fundus when the affected person is examined within the left lateral decubitus place. Fixed stones in the gallbladder neck are regularly associated with cholecystitis. If large stones or a number of stones fill the whole gallbladder lumen, there may be little surrounding bile. When this occurs, gallstones are recognized by the "wall echo shadow" signal produced by echoes from the anterior gallbladder wall, echogenic anterior floor of the stone, and posterior acoustic shadowing produced by the stone. Sludge will change with positional variation and strikes slowly, whereas gallstones roll shortly on real-time ultrasound. The gallbladder is finest evaluated when distended, and subsequently patients ought to fast earlier than the scan. Cholecystitis Acute cholecystitis (see Chapter 33) is due to obstruction of the cystic duct or gallbladder neck, often by a gallstone. The gallbladder becomes distended with a chemical irritation of the mucosa, producing a tense and tender gallbladder with wall edema and irritation. A, Normal longitudinal gallbladder picture with visualization of the gallbladder neck. Ultrasound findings of acute calculous cholecystitis embody gallstones, gallbladder wall thickening higher than three mm, pericholecystic fluid, and a constructive sonographic Murphy sign. In emphysematous cholecystitis, echogenic air bubbles in the gallbladder wall produce reverberation artifact. Gangrenous cholecystitis occurs extra usually in patients with diabetes mellitus or a white blood cell rely higher than 15,000 cells/mL (Fagan et al, 2003). Ultrasound features of gangrenous cholecystitis include floating intraluminal membranes from sloughed mucosa, shadowing foci from air within the gallbladder wall, disrupted gallbladder wall, and pericholecystic abscess formation (Jeffrey et al, 1983). Gallbladder wall thickening is nonspecific and may be seen in a variety of gallbladder disease and extracholecystic pathologic circumstances. Diffuse gallbladder wall thickening in patients with out major gallbladder wall disease occurs in quite lots of systemic processes, such as hypoalbuminemia, congestive coronary heart failure, hepatitis, and pancreatitis (van Breda Vriesman et al, 2007). A, Longitudinal view of the gallbladder reveals layering stones (numbered) with acoustic shadow. Hyperplastic Cholecystoses and Gallbladder Polyps Hyperplastic cholecystoses (see Chapter 49), such as cholesterolosis and adenomyomatosis, may cause focal or polypoid gallbladder wall thickening. Cholesterolosis results from irregular ldl cholesterol deposits in the gallbladder wall creating wall irregularities or polypoid intraluminal masses. Cholesterol polyps are benign with no malignant potential (Ito et al, 2009; Levy et al, 2002; Terzi et al, 2000). Adenomyomatosis is a benign hyperplastic cholecystosis with no malignant potential that outcomes from hyperplasia of both the mucosa and muscularis propria of the gallbladder wall. The majority of incidentally detected polypoid gallbladder lesions are nonneoplastic and characterize ldl cholesterol polyps or inflammatory polyps (Corwin et al, 2011). Rarely, these could additionally be neoplastic, similar to adenomas, and malignant transformation to adenocarcinoma is a concern. Adenomas are inclined to be solitary and uniformly hyperechoic but turn into extra heterogeneous as they improve in dimension and will either be pedunculated or sessile. In patients with polypoid gallbladder lesions, risk elements for malignancy include age of patient (> 60 years of age), coexistence of gallstones, and dimension of the polypoid lesion (>10 mm in diameter) (Terzi et al, 2000). The prevalence of malignancy in polyps larger than 10 mm ranges from 37% to 88% (Ishikawa et al, 1989; Koga et al, 1988). A, Longitudinal sonogram exhibits a distended gallbladder with thickened irregular wall(arrows) and layering sludge(arrowheads). Often, asymptomatic gallbladder polyps smaller than 10 mm are followed sonographically, and people smaller than 6 mm will not be adopted or followed at prolonged intervals (Pedersen et al, 2012). Secondary signs of gallbladder most cancers embody discontinuity of the echogenic mucosal lining, absence of echogenic specks seen in cholesterol crystals, and highvelocity arterial move higher than 60 cm/s. In the era of laparoscopic surgery for gallstone illness, it may be very important assess the gallbladder rigorously on preoperative ultrasound to exclude occult gallbladder cancer and to plan an appropriate surgical strategy. Approximately 47% of gallbladder carcinomas are detected by the way at laparoscopic cholecystectomy (Duffy et al, 2008). On imaging, you will want to show the reference to the bile ducts to differentiate this situation from polycystic illness. Arterial indicators from the fibrovascular bundle at the margin of the saccules may also aid in prognosis (Miller et al, 1995). Biliary Obstruction Measurement of the extrahepatic duct is usually performed near the crossing of the hepatic artery, with measurement of the lumen from inside wall to inside wall. There could also be no change or solely a slight improve in diameter after cholecystectomy (Abbitt, 2002; Feng & Song, 1995; Mueller et al, 1981). Variable threshold values in literature are due to differences in sample measurement, patient population, and control of confounding variables. Intrahepatic ducts should measure larger than 2 mm or higher than 40% of the adjoining portal vein to be considered dilated. Intrahepatic bile duct dilatation is greatest appreciated in transverse images of the left hepatic lobe. To decide the extent of obstruction, the left and proper primary ducts are adopted transversely to their junction, and transverse views of the frequent hepatic and common bile ducts are obtained. Calculi could form or reflux into the intrahepatic ducts, and small calculi can be mistaken for air (see Chapters 36 and 37). Transabdominal ultrasound stays operator dependent, however, when carried out by skilled examiners, has excessive diagnostic accuracy for choledocholithiasis (Rickes et al, 2006). Hemobilia could layer or seem echogenic and masslike if the clot is organized (see Chapter 125). A, Mass (m) obstructs a mildly dilatedcommonbileduct(arrows)andinvolvesthemainportalvein(v). Obstruction as a outcome of biliary ascariasis is related to tubular constructions inside the bile duct, and motion of the worms is pathognomonic (Lim, 1990). Pancreatic carcinoma, gallbladder carcinoma, and cholangiocarcinoma can all cause biliary dilatation. The sample of biliary obstruction and the appearance of the duct wall are also useful for prognosis. Recurrent pyogenic cholangitis is evidenced by dilated ducts with intraductal calculi and segmental dilatation, incessantly in the left lobe (see Chapter 39). Primary sclerosing cholangitis causes a beaded look of the ducts with wall thickening, strictures, and discontinuous areas of dilatation; intraluminal echoes within the dilated ducts represents particles such as pus, sludge, or sloughed epithelium (see Chapter 41). For tumors adjacent to the umbilical portion of the left portal vein, delicate bile duct dilatation or wall thickening could also be a clue to biliary ductal involvement. Cholangiocarcinoma Cholangiocarcinoma is a ductal tumor of the intrahepatic or extrahepatic bile ducts (see Chapter 47).
References
- Cardinale D, Colombo A, Lamantia G, et al. Anthracycline- induced cardiomyopathy: clinical relevvance and response to pharmacologic therapy. J Am Coll Cardiol 2010;55:213-220.
- Granger CB, McMurray JJ, Yusuf S, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensinconverting-enzyme inhibitors: the CHARM Alternative trial. Lancet. 2003;362(9386):772-776.
- Takeshita S, Tokutomi T, Kawase H, et al: Elevated serum levels of matrix metalloproteinase-9 (MMP-9) in Kawasaki disease, Clin Exp Immunol 125(2):340-344, 2001.
- Root HD, Keizer PJ, Perry JF, Jr: The clinical and experimental aspects of peritoneal response to injury. Arch Surg 95:531-537, 1967.
- Gockel I, Junginger T, Bernhard G, et al: Heller myotomy for failed pneumatic dilation in achalasia: How effective is it? Ann Surg 239:371, 2004.
- Argenziano M, Katz M, Bonatti J, et al. Results of the prospective multicenter trial of robotically assisted totally endoscopic coronary artery bypass grafting. Ann Thorac Surg. 2006;81: 1666-74.

