Suhagra
Curtis Sheldon, MD
- Assistant Professor of Surgery, University of Cincinnati
- Director, Pediatric Urology, Cincinnati Children’s Hospital,
- Cincinnati, Ohio
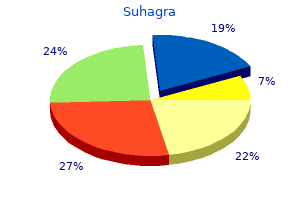
Suhagra dosages: 100 mg, 50 mg
Suhagra packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

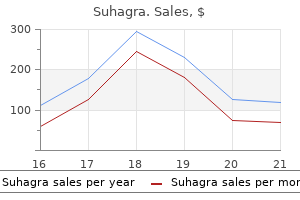
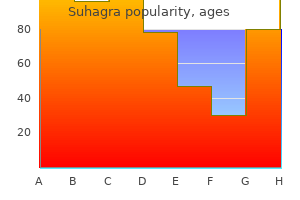
Purchase suhagra 50mg
The latissimus muscle could also be elevated off the chest wall as needed for tumor resection impotence definition inability order suhagra 100mg line. Chest wall involvement could require thoracotomy and resection of contiguous ribs; deflate the lung earlier than opening the chest cavity to defend the underlying lung erectile dysfunction treatment singapore discount suhagra 100mg with amex. Intrathoracic extent of tumor could also be determined by palpation of the pleural floor following thoracotomy erectile dysfunction pump order suhagra 50 mg overnight delivery. Osteotomy of the ribs using a rib cutter underneath direct visualization permits en bloc elimination of the involved chest wall. Reconstruction Following Tumor Resection Repair and reconstruction of the axilla is necessary following tumor resection. Insertion of an epineural catheter into the sheath of the brachial plexus permits postoperative administration of local anesthetics similar to bupivacaine (Marcaine) to reduce postoperative ache. Extremely giant, low-grade, fibrosarcoma of the axilla extending from the thoracic outlet to the posterior axillary line and to the level of the breast. All tissues were eliminated through a mix of the anterior and posterior parts of the utilitarian shoulder girdle incision. Intraoperative photograph taken earlier than reconstruction and reattachment of the muscles of the again and anterior pectoralis main. This photograph demonstrates the advantage of a transpectoralis approach anteriorly mixed with a posterior strategy. Reattachment of the conjoint tendon and pectoralis minor to the coracoid with using mattressed, nonabsorbable sutures covers the brachial plexus and axillary vessels. Defects of the chest wall can be lined with local rotation flaps utilizing the latissimus dorsi or pectoralis main muscle, which may be tenodesed to the subscapularis tendon as needed. Careful wound closure over closed suction drains and placement of absorptive padding within the axilla scale back the chance of pores and skin maceration and wound infection. Functional deficits ensuing from resection of parts of the brachial plexus may require delayed reconstruction after completion of adjuvant treatment. Detachment of the humeral insertion is essential to opening up the entire axilla and permits exploration of all necessary buildings. Injury as a end result of over-retraction of the conjoint tendon may occur, leading to loss of elbow flexion and resulting incapacity. Operative view through the anterior incision displaying a big tumor surrounding the axillary sheath. Lymphedema might result in important disability and chronic ache; early aggressive remedy might lessen the severity or length of swelling. Infections and flap necrosis following axillary tumor resections rarely happen, because of the substantial network of subcutaneous blood vessels perfusing the shoulder girdle. Upper extremity limb salvage with microvascular reconstruction in patients with advanced sarcoma. Upper extremity reconstruction following resection of sentimental tissue sarcomas: a functional outcomes evaluation. Soft tissue sarcoma of the higher extremity: a 5-year experience at two institutions emphasizing the role of soppy tissue flap reconstruction. Cost analysis of useful restoration surgical procedure for extremity soft-tissue sarcoma. Loss of shoulder movement leads to mild incapacity, which is definitely compensated for by use of the other arm for overhead actions. Use of nerve sheath catheters with postopera Chapter 14 Forequarter Amputation Jacob Bickels and Martin M. Forequarter amputation normally is contraindicated when the tumor extends to the chest wall or to the posterior triangle of the neck and paraspinal muscular tissues. This surgical procedure may be thought-about in chosen cases with no metastases, in which concomitant chest wall resection or neck dissection can obtain negative margins and patients can face up to the physiologic impact of those combined main surgical procedures. All of these should be transected to allow the performance of a forequarter amputation. The axillary vessels and infraclavicular portion of the brachial plexus cross just inferiorly to the coracoid course of, which is easily palpable, and lie under the deltopectoral fascia. These constructions must be evaluated earlier than surgery to determine the phase that could be safely transected and ligated, particularly as a outcome of giant tumors may come near the thoracic outlet. Large tumors of the periscapular space could easily prolong into the posterior triangle of the neck, the adjoining paraspinal muscle tissue, and the underlying chest wall. Tumor extension into these anatomic sites must be evaluated fastidiously before surgical procedure in case en bloc resection of a chest wall section or a concomitant neck dissection is required. Angiography is extremely useful in finding the anatomic place of the axillary and brachial vessels, and in evaluating whether these buildings are concerned by tumor. Physical anomalies (eg, a replica axillary artery) occasionally are identified as well. Angiography also makes it potential to determine precisely the most effective degree of ligation of the axillary vessels. No imaging studies can distinguish precisely whether or not the brachial plexus is infiltrated by tumor or whether or not the vessels and plexus are merely displaced, and they present solely oblique proof of tumor extension to the nerves. On the other hand, venography of the axillary veins is a simple and accurate methodology of figuring out brachial plexus involvement. Large bone tumor (primary bone sarcoma or metastatic lesion) of the proximal humerus and scapula with and extensive soft tissue part and invasion into the shoulder joint and surrounding muscles. An axillary roll is placed beneath the axilla to allow full tour of the chest, and a sponge-rubber pad is positioned beneath the hip to prevent ischemic damage to the skin in this space. Forequarter amputation entails en bloc removal of the higher extremity along with the scapula and the lateral facet of the clavicle. The most common indications embody massive sarcomas or carcinomas of the axillary house with involvement of the bony shoulder girdle or tumor fungation by way of the axilla. Lymphoma of the shoulder girdle and brachial plexus with a non-union pathological fracture and no response to radiation remedy. Plain radiograph exhibiting destruction of the proximal humerus and the shoulder joint, as well as a non-union fracture. Plain radiograph demonstrating very massive soft tissue mass within the axillary area brought on by extraosseous growth of a Ewing sarcoma. The neurovascular bundle was encased and compressed by the tumor, and the patient had overt edema of the upper extremity and compromised radial and median nerve functions. Axillary venography showing that the axillary vein is nearly utterly thrombosed from compression by surrounding tumor. This appearance has proven to be an especially dependable prognostic finding of brachial plexus involvement. If axillary venography exhibits axillary vein obstruction, a forequarter amputation almost is all the time required on the time of exploratory surgery. The affected person is placed in a full lateral place and is secured to the working table on the hips with tape. An axillary roll is positioned underneath the axilla to allow full excursion of the chest, and a spongerubber pad is placed beneath the hip to prevent ischemic injury to the skin in this space. Intraoperative pictures exhibiting a domestically recurrent osteosarcoma at the proximal arm and axilla in a 34-year-old patient E.
Buy 100mg suhagra mastercard
Kjaer-Petersen and colleagues11 discovered that erectile dysfunction treatment for heart patients suhagra 100mg sale, no matter remedy best pills for erectile dysfunction yahoo best 100mg suhagra, long-term symptoms have been current in 38% of sufferers at four doctor of erectile dysfunction 50 mg suhagra for sale. Petrie and Lamb,thirteen who used immediate, unrestricted motion, reported on outcomes at four. Another study found that pain was related to the degree of posttraumatic arthritis secondary to articular incongruity and advocated anatomic reductor and inside fixation. Tendon arthroplasty of the fifth carpometacarpal joint for therapy of posttraumatic arthritis. Intra-articular fractures on the base of the fifth metacarpal: a medical and radiographical examine of 64 circumstances. Clinical results of intraarticular fractures of the bottom of the fifth metacarpal treated by closed reduction and cast immobilization. Dislocated intra-articular fracture of the bottom of the fifth metacarpal: a clinical research of 23 patients. Proximal fractures of the fifth metacarpal: a retrospective evaluation of 25 operated instances. The therapy of metacarpal fractures affects finger function and must be weighed against the sequelae of the fracture itself. The adjacent lateral furrow or so-called collateral recess permits passage of the interosseous tendon and should function a portal of entry for Kirschner wire fixation into the intramedullary canal. The metacarpal less generally is injured by a crush-type injury that flattens the metacarpal arch bridging the carpus to the phalanges. Crush accidents typically involve a number of metacarpals and are often associated with different fractures and vital gentle tissue trauma. As with different long tubular bones, the precise sample is determined by the diploma of shear and torsion related to the utilized load. The fracture usually has apex-dorsal malalignment secondary to the flexion drive applied by the lumbrical and interossei muscular tissues. When severely disrupted, the muscles have the potential for disabling scarring and "intrinsic contracture. A Extensor tendons Extensor tendon Collateral ligament and capsule of the metacarpophalangeal joint Collateral recess Interosseous m. Each metacarpal crosssection is roughly triangular, with intrinsic musculature on either side and the extensor tendon on the dorsal floor. Low-energy transverse or indirect fractures of a single metacarpal often keep acceptable alignment and heal without any measurable useful deficit. Spiral fractures, comminuted fractures, and fractures of a quantity of metacarpals are extra likely to shorten and rotate, leading to tendon imbalance and overlapping of the fingers. Fractures of the metacarpal neck (usually the fourth or fifth) might have varying degrees of apex-dorsal malalignment. Flexion of the fourth or fifth metacarpal heads past 30 and forty five degrees, respectively, leads to a visible pseudoextensor lag and sometimes pain in the palm throughout greedy. The examiner should visualize the fingers as the affected person carries them via an arc of movement. The examiner should decide the diploma of dorsal fracture eminence or palmar metacarpal head prominence. These injuries should be treated urgently with surgical d�bridement before infection develops. Carpal tunnel and compartment syndromes: High-energy fractures might end in compartment syndrome, necessitating fasciotomy of the involved intrinsic muscle tissue. Carpal tunnel syndrome can also result, notably with an related wrist damage corresponding to a perilunate dislocation. Traction views could also be carried out to assess the degree of comminution at the fracture site or to examine the mobility of subacute fractures. Apex-dorsal malalignment of the border metacarpals could also be partially corrected with discount and splinting. While distracting at the fracture site, upward drive is applied to the proximal phalanx and metacarpal head to realign the neck and shaft. A splint with three-point molding is utilized with dorsal compression on the fracture site and volar assist for the metacarpal head and base. Percutaneous surgical methods are sometimes adequate for lowenergy metacarpal shaft fractures and for most metacarpal neck fractures. Open discount and internal fixation ought to be considered for open fractures, shaft fractures with vital comminution, and fractures associated with joint disruption, tendon harm, or neurovascular damage. Crush-type injuries flatten the bony arch of the hand, often leading to open metacarpal neck fractures with various degrees of soppy tissue injury. The dorsal soft tissues are often tenuous and surgical incisions can outcome in necrosis and the necessity for in any other case pointless delicate tissue coverage procedures. Metacarpal fractures resulting from projectiles are graded as either low or excessive energy. Oblique view of the hand demonstrates fourth and fifth metacarpal shaft fractures. Long indirect fractures of the fourth and fifth metacarpal heads have been stabilized with a quantity of lag screws. An adjacent transverse fracture of the ring finger proximal phalanx has been repaired with a plate. Clinical photograph of a crushed hand reveals international swelling and splitting of the skin indicative of extreme inside degloving. Fractures are stabilized with percutaneous pins to avoid extra trauma from surgical dissection. Callus often varieties because the fracture fragments, although comminuted, remain vascularized. Provisional fixation with Kirschner wires may be thought-about if serial d�bridements are anticipated. Simple thumb metacarpal shaft fractures usually heal in acceptable alignment with nonoperative administration. For example, a grossly contaminated and devitalized open metacarpal fracture may be handled with percutaneous Kirschner wires to reduce additional delicate tissue stripping. In distinction, a easy closed transverse metacarpal fracture in a dentist would be thought of for dorsal plating to facilitate a immediate return to work. A surgeon facile with the strategy of collateral recess pinning could quickly stabilize multiple metacarpal fractures. Poorly placed percutaneous wires in any approach could trigger extra gentle tissue issues (eg, infection) than open discount and fixation. A radiograph of the hand exhibits percutaneous fixation of displaced metacarpal fractures from a gunshot wound. A locking plate utilized with cancellous bone graft to fill the void resulted in stable healing. Fractures of the first ray, as shown in this radiograph, usually result in contraction of the thumb�index net house. A medical photograph reveals application of an external fixator to permit fracture consolidation in a practical place. A single extra-articular metacarpal fracture is approached with a dorsal longitudinal incision.

Buy suhagra 50 mg with amex
The gel freezes and creates an ice ball within a few seconds after perfusion of the argon fuel through the probe impotence penile rings suhagra 50 mg mastercard. It would have been tough to freeze these websites with direct pour of liquid nitrogen as a outcome of impotence webmd generic suhagra 100mg the relatively large dimension of the B funnels erectile dysfunction juice drink buy cheap suhagra 50 mg. Patients with lesions of the lower extremities are stored non�weight bearing for six weeks. Plain radiographs are then obtained to rule out fracture and establish bone graft incorporation. It would have been tough to obtain such a variety and muscle energy after the resection of the distal femur that in any other case would have been supplied to this affected person. This potential downside initially was underestimated by surgeons who pioneered the applying of this technique in scientific practice. Inadequate protection of sentimental tissues, lack of mechanical fixation, and failure to use perioperative antibiotics resulted in unacceptably excessive rates of fractures, delicate tissue damage, infections, and neurapraxias. As a end result, the same authors reported a later series of patients with a considerably decreased rate of these problems. They had been thought-about pathological as a result of they occurred via a mechanically weakened bone and following a minor trauma. Infections and flap necrosis even have become rare issues because of mobilization and safety of soft tissues previous to freezing and the use of perioperative antibiotics. When the latter do occur, the neurologic damage normally is transient and heals spontaneously. Cryoablation also was shown to be related to minimal harm to the adjacent articular cartilage, with degenerative changes reported in lower than 3% of instances in a large collection of patients. Plain radiograph showing pathological fracture of the proximal tibia following cryoablation and on weight bearing. Reconstruction following cryoablation in that patient consisted of autologous bone graft solely. The wide collapse and destruction of the articular surface made resection of the proximal tibia and reconstruction with endoprosthesis inevitable. This complication is rare when adequate padding and warming with saline are carried out. Any compromise of both of these criteria ultimately may end in local tumor recurrence. Better case choice, adequate curettage, and meticulous burr-drilling have led to a drop in local recurrence charges, to lower than 5% in most series. Although a lot of the fuel exits into the atmosphere by way of the surgical wound, a substantial quantity nevertheless is pushed into the pulmonary circulation beneath the influence of the strain brought on by boiling of liquid nitrogen in the bony cavity, and exhaled. Treatment of huge subchondral tumors of the knee with cryosurgery and composite reconstruction. Recurrent aneurysmal bone cyst of the proximal phalanx treated with cryosurgery: a case report. Tissue impedance and temperature measurements in relation to necrosis in experimental cryosurgery. Effect of hypertonic stress on mammalian cell traces and its relevance to freeze-thaw harm. Cryosurgery in long bones: an experimental research of necrosis and revitalization in rabbits. Cryosurgery and acrylic cementation as surgical adjuncts in the therapy of aggressive (benign) bone tumors: evaluation of 25 patients under the age of 21. The impact of cryosurgery and polymethylmethacrylate in dogs with experimental bone defects corresponding to tumor defect. Giant cell tumor and aneurysmal bone cyst of the talus: clinicopathological review and two case stories. Cryosurgery in the remedy of solitary or a number of bone metastases from renal cell carcinoma. Conservative surgery for giant cell tumors of the sacrum: the function of cryosurgery as a supplement to curettage and partial excision. Cryosurgery within the remedy of giant cell tumor of bone: a report of 52 consecutive cases. Eosinophilic granuloma of bone: results of remedy with curettage, cryosurgery, and bone grafting. Treatment of benign and low-grade malignant intramedullary chondroid tumours with curettage and cryosurgery. Clinical outcomes of the momentary acrylic bone cement plug in the treatment of bone tumors: a multicentric research. The scapula and proximal humerus are common sites of major sarcoma, including osteosarcoma and Ewing sarcoma in kids and chondrosarcoma in adults. Metastatic tumors, particularly hypernephroma, also will be inclined for the proximal humerus. When soft tissue tumors happen within the upper extremity, they have a tendency to favor the shoulder girdle and will secondarily contain the scapula, proximal humerus, or clavicle. The axilla is one other site across the shoulder girdle where major soft tissue tumors might develop or where metastases can unfold to and exchange the native lymph nodes. The axilla is a comparatively "silent" space, where tumors may grow to giant sizes earlier than they turn into symptomatic and are detected. The shoulder girdle consists of the proximal humerus, the scapula, and the distal third of the clavicle, as nicely as the encompassing gentle tissues. Each bone could additionally be involved by a major malignant bone tumor or metastases, with or without delicate tissue extension. Until the mid-20th century, forequarter amputation was the remedy for malignant tumors of the shoulder girdle. Today, about 95% of sufferers with sarcomas of the shoulder girdle can be treated safely by limb-sparing resection such as the Tikhoff�Linberg resection and its modifications. The resection and reconstruction of tumors of the shoulder girdle consists of three elements: (1) surgical resection of the tumor following oncologic rules; (2) reconstruction of the skeletal defect (ie, endoprosthetic replacement); and (3) delicate tissue reconstruction utilizing a quantity of muscle transfers to cover the skeletal reconstruction and provide a practical extremity. The targets of all shoulder girdle reconstructions are to provide a stable shoulder and to protect regular elbow and hand perform. The extent of tumor resection and remaining motor teams out there for reconstruction dictate the diploma of shoulder motion and function that are retained. Historical Background Some of the earliest discussions regarding limb-sparing surgical procedure targeted on techniques for resection of tumors about the scapula. Initial reviews of shoulder girdle resections have been confined to the individual bones or portions of the scapula. The first reported scapular resection was a partial scapulectomy performed by Liston in 18197 for an ossified aneurysmal tumor. Between this time and the mid-1960s, several other authors mentioned limb-sparing resections concerning the shoulder girdle.
Buy suhagra 100mg on line
No single imaging study is available that precisely visualizes the brachial plexus erectile dysfunction doctor el paso buy discount suhagra 100 mg online. Venography erectile dysfunction treatment wikipedia buy suhagra 50 mg low price, however erectile dysfunction doctors buffalo ny order 50mg suhagra with amex, is extraordinarily correct in predicting brachial plexus invasion. The axillary vein, axillary artery, and brachial plexus journey in intimate association inside a single fascial sheath, the axillary sheath. The main nerves and cords travel alongside the periphery of the sheath; subsequently only full obliteration-not simply compression-of the brachial or axillary vein denotes direct tumor extension in and across the nerves and likewise indicates secondary involvement of the venous wall. This development additionally explains the clinical triad of ache, motor loss, and venous obstruction. In these situations arteriography demonstrates displacement of the axillary artery; nevertheless, the axillary artery remains patent due to its thick partitions and excessive intraluminal pressures. The last decision regarding the need for a forequarter amputation should be reserved until surgical exploration of the brachial plexus has been carried out. Prosthetic Reconstruction When endoprosthetic reconstruction was developed in the 1940s, consideration initially was focused on reconstruction of skeletal defects of the lower extremity. Use of the technique was broadened steadily to embody defects of the higher extremity and shoulder girdle. Reported charges of fracture, infection, nonunion, reoperation, and tumor recurrence are lower, and size of immobilization is shorter with extremity endoprosthetic reconstruction than with allograft, composite reconstruction, or arthrodesis. A large soft tissue axillary tumor protruding anteriorly through the pectoralis major and the skin. Angiography and embolization of metastatic renal cell carcinoma (hypernephroma) to the distal clavicle. Embolization typically is carried out for large high-grade soft tissue sarcomas previous to a resection. This is the most pathognomonic finding of brachial plexus involvement seen during the time of surgery. Brachial plexus involvement often correlates with the clinical findings of neurologic deficits, numbness, or muscle weak spot of the affected extremity. Soft tissue reconstruction is accomplished utilizing a dual suspension method that employs static and dynamic methods of prosthetic stabilization and delicate tissue and motor reconstruction. This technique offers secure fixation and stabilization of the prosthesis until the soft tissues heal and scar to each other. Dynamic methods of stabilization and reconstruction include a quantity of muscle rotation flaps and muscle transfers that eventually heal, scar to one another and the prosthesis, and supply the mandatory motor units for a useful extremity. Soft tissue reconstruction follows skeletal reconstruction and static stabilization. The brief head of the biceps is connected with a tenodesis proximally to the coracoid (intra-articular proximal humerus reconstruction), or to the clavicle (extra-articular proximal humerus reconstruction) or pectoralis main (total scapula reconstruction). The pectoralis minor also is tenodesed again to its origin, when potential, or to the scapula to protect the neurovascular buildings. The pectoralis major is repaired to its humeral insertion or, in cases requiring extraarticular proximal humerus reconstruction, transferred to cover the prosthesis with soft tissues. The latissimus dorsi may be transferred laterally to function as an exterior rotator following extra-articular proximal humerus resection. In complete scapula reconstruction, the periscapular muscles are tenodesed to the prosthesis with heavy nonabsorbable sutures or tapes in a way that covers the whole prosthesis with muscle. Following isolated axillary tumor resection, the distal (humeral) transected edge of the latissimus dorsi muscle is rotated into the defect and sutured to the superficial floor of the subscapularis muscle to fill the dead house. This incision has been developed based on the intensive experience of surgeons performing resections across the shoulder girdle. Dashed line A indicates the anterior strategy, an prolonged deltopectoral incision coming from the midclavicle via the deltopectoral interval and distally over the medial side of the arm, curving in a posterior course. This permits resection of huge axillary tumors or performance of forequarter amputations. The preliminary steps of the anterior approach of the utilitarian shoulder girdle incision. The key to this approach is the discharge of the pectoralis major from its insertion on the humerus (1�2 cm away). With the pectoralis main now mirrored onto the chest wall, the whole axillary house can be uncovered. With the pectoralis main layer retracted, the axillary house is completely coated by fascia, much like the peritoneum. This covers two muscular tissues, the quick head of the biceps and the pectoralis minor, which connect to the coracoid course of, which should be released. With these two muscle tissue released, the axillary area and infraclavicular element of the brachial plexus (ie, the axillary vein and artery by way of its complete length) may be explored completely. If essential, a portion of the clavicle can be resected to uncovered the subclavian artery and vein. Chronic swelling in the distal extremity, intractable ache, motor loss, and a venogram that demonstrates obliteration of the axillary vein strongly counsel that the tumor is unresectable. The final determination regarding the necessity for a forequarter amputation is made intraoperatively, after anterior publicity and exploration of the brachial plexus and neurovascular constructions. Neurovascular exploration and mobilization Type of resection the necessary thing to a safe and adequate resection of all types of neoplasms around the shoulder girdle lies in sufficient visualization, publicity, dissection, mobilization and preservation of all vital neurovascular constructions. Full exposure is facilitated by releasing the pectoralis major muscle from its humeral insertion and the strap muscles from the coracoid course of. High-grade sarcomas that come up from the proximal humerus or scapula are more likely to contaminate or cross the glenohumeral joint, either grossly or microscopically. An extra-articular type of resection is used for many high-grade sarcomas arising from the scapula or proximal humerus. Soft tissue reconstruction Soft tissue reconstruction is just as necessary as skeletal reconstruction during limb-sparing surgery if a useful extremity is to be offered. Static and dynamic methods of sentimental tissue reconstruction and stabilization are used. Static methods rely on heavy nonabsorbable sutures, Dacron tapes, and Gore-Tex grafts. Survival charges based on Kaplan�Meier evaluation show a 9-year survival fee of 98% to 99% for proximal humeral replacements. Other teams have reported a significant incidence of dislocation following endoprosthetic reconstruction of the shoulder girdle, however this has not been our expertise. The pectoralis main has been detached from the clavicle, and the deltoid has been detached from the acromion. Composite photograph demonstrating head, body, and stem elements for humeral resections.

Purchase suhagra 100mg with visa
Lesions which have triggered extensive destruction and violated that continuity what food causes erectile dysfunction 100mg suhagra visa, nonetheless erectile dysfunction drugs bayer order suhagra 50mg line, require intercalary resection of the humeral diaphysis latest advances in erectile dysfunction treatment buy suhagra 100mg online. Most of the cortical diameter was destroyed, and even the remaining posterior cortex had been infiltrated and thinned by the disease, so distal femur resection with endoprosthetic reconstruction was carried out. Extensive and damaging metastasis of proximal femur, which leaves no choice however resection of the proximal femur and reconstruction with prosthesis. Reconstruction should present quick stability that must not rely on biologic therapeutic processes. Reconstruction ought to embrace the combined use of hardware or prosthetic implants and bone cement (ie, polymethylmethacrylate). The latter is used to reinforce the hardware by growing the diameter of the assemble via which the mechanical load is transmitted and bettering its attachment to the neighboring bone, thereby allowing the assemble to with- stand the mechanical stresses of instant weight bearing and performance. Adjuvant Radiation Therapy Postoperative external-beam radiation remedy of 3000 to 3500 Gy routinely is administered to the complete surgical field to control remaining microscopic disease. Resection of such tumors at the proximal humerus would require en bloc removing of the overlying deltoid muscle, the rotator cuff tendons, and the joint capsule. Bone metastases, nonetheless, normally present with less in depth soft tissue involvement, and their resection entails removal of bony parts with only a thin layer of surrounding soft tissues. This process is straightforward to perform, but it could fail, because tumor development leaves the nail as the only load-transmitting component of the decrease extremity, ultimately resulting in hardware failure and breakage. Plain radiograph exhibiting an impending fracture of the femoral diaphysis because of a quantity of myeloma. Tumor removal, cemented nailing, and postoperative radiation more than likely would have resulted in local tumor control and durable reconstruction. Closed nailing was done on this patient, however, and tumor development (despite radiation) resulted in unavoidable hardware G breakage. Similar end result with uncemented fixation of metastatic renal cell carcinoma of the subtrochanteric region. Surgery should include meticulous tumor removal and filling of the whole tumor cavity with bone cement. Function after resection of humeral metastases: evaluation of 59 consecutive patients. Impending and precise pathological fractures in sufferers with bone metastases of the long bones: a retrospective research of 233 surgically handled fractures. Impending pathologic fractures from metastatic malignancy: evaluation and administration. Comparison between solitary and multiple skeletal metastatic lesions of breast most cancers patients. Metastatic disease in lengthy bones: a proposed scoring system for diagnosing impending pathologic fractures. Surgical therapy of skeletal metastatic lesions of the proximal femur: endoprosthesis or reconstruction nail A study of the surgical treatment of 166 pathological humeral and femoral fractures. Chapter 6 Cryosurgical Ablation of Bone Tumors Jacob Bickels, Isaac Meller, Yehuda Kollender, and Martin M. Cryoablation performed by direct pouring of liquid nitrogen is an efficient adjuvant to curettage in the administration of a big variety of bone tumors, together with benign�aggressive, metastatic, and primary malignant lesions. It is an intralesional process, which permits the avoidance of major resection and associated loss of perform. It weakens the bone surrounding the tumor cavity and, when not used judiciously, might cause extra soft tissue accidents. Awareness of these potential issues has led to refinement of surgical practices to embrace gentle tissue protection, stable reconstruction, the utilization of perioperative antibiotics, and enhancement of rehabilitation protocols for gradual weight bearing. Those tips have resulted in a gratifyingly low price of problems and rendered this treatment a protected and dependable modality. Historical Aspects and Physiologic Background Although cryoablation had been used in the 1850s for the management of domestically advanced carcinoma of the cervix, its applicability to the management of bone tumors was not assessed until more than a century later, within the traditional 1966 animal research by Gage et al,13 during which the femora of dwelling mongrel dogs had been frozen by perfusing liquid nitrogen via encircling latex coils. Liquid nitrogen, which has a boiling temperature of 196�C, allowed speedy freezing of a 2-cm rim of bone around these coils. Using histopathologic research and plain radiographs, the authors documented the occurrence of tissue necrosis and bone resorption that was associated with mechanical weakening and spontaneous fractures. They additional advised using intralesional cryoablation in lieu of tumor resection or amputation. Further studies confirmed and refined the initial findings of Gage et al13 and confirmed that temperatures between 21�C and 60�C are wanted to acquire cell necrosis; temperatures below 60�C exerted no further lethality. Four mechanisms are concerned in the quick cytotoxicity produced by cryoablation: (1) formation of ice crystals and membrane disruption; (2) thermal shock; (3) dehydration and toxic effects of electrolyte adjustments; and (4) denaturation of cellular proteins. The formation of intracellular ice crystals is considered as being the principle mechanism of quick mobile necrosis. The withdrawal of water from the system into these crystals creates a hyperosmotic extracellular environment, which, in flip, attracts water from the cells. As the process continues, these crystals grow, the cells shrink and dehydrate, electrolyte focus is increased, and membranes and cell constituents are damaged. Histologically, essentially the most dramatic effect of cryoablation is on the appearance of the bone marrow: a rim of 1 to 2 cm of extensive necrosis with minimal inflammatory response appears following direct pour of liquid nitrogen. A large cortical window the dimensions of the longest longitudinal dimension of the tumor is made after exposure of the involved bone. The neurovascular bundle and fasciocutaneous flaps are protected by mobilization and by shielding (with surgical pads) from direct contact with the liquid nitrogen, after which cryoablation is carried out. The tumor website is extensively uncovered by a deltopectoral incision, and fasciocutaneous flaps are mobilized to expose the whole extent of the tumor. A massive cortical window the size of the longest longitudinal dimension of the tumor is made. This must be meticulously carried out, leaving only residual microscopic disease within the tumor cavity. Thermocouples are used to monitor the freeze within the cavity, cavity wall, adjoining delicate tissues, and an area 1 to 2 mm from the periphery of the cavity. The surrounding delicate tissues are irrigated repeatedly with heat saline resolution to decrease the potential for thermal damage. Freezing (boiling of liquid nitrogen) lasts 1 to 2 minutes and is proportional to the quantity of poured liquid nitrogen. The cycle is considered complete as soon as the temperature of the cavity rises above 0�C. The cavity is irrigated with saline after two freeze�thaw cycles have been carried out. Direct pour of liquid nitrogen into the tumor cavity, which is irrigated repeatedly with warm saline throughout the freezing and thawing processes (5 minutes altogether).
Suhagra 50 mg line
Proximal femur and proximal humerus replacements have probably the most superior survival results erectile dysfunction gene therapy quality 50mg suhagra, adopted by distal femur erectile dysfunction at 55 cheap suhagra 100 mg mastercard, and then proximal tibia erectile dysfunction hypothyroidism cheap 100mg suhagra otc. Kaplan-Meier survival curve exhibiting superior results of modular substitute system when in comparability with customized prostheses over all anatomic sites. Today, more endoprosthetic reconstructions are performed for non-oncologic reconstructions than for osteosarcomas. Ongoing analysis continually strives to enhance the result following endoprosthetic reconstruction. Continued work on improved metallurgy and polymers, significantly with the introduction of cross-linked polyethylene, guarantees improved long-term sturdiness. Routine use of premixed antibiotic cement and experimentation with antimicrobial implant surfaces may assist to reduce the danger of periprosthetic an infection. New methods for tendon attachment to the prosthesis include novel clamps and ingrowth surfaces to promote improved junctional energy. New implant technologies such because the Rephyisis noninvasive expandable prosthesis supply hope to younger youngsters with few various choices. New fixation strategies, including hydroxyapatite stems with porous coated surfaces, could additionally be of great worth in non-oncologic patients. The lately launched Compress system represents the first new technique of prosthetic fixation in a long time. We have already adapted this system to increase the applicability of intercalary endoprosthetic reconstruction. Although future advances in tissue engineering maintain the promise of artificially engineered living bone, we anticipate that endoprosthetic reconstruction will stay the preferred choice of orthopaedists for a few years to come. Reconstruction utilizing the saddle prosthesis following excision of major and metastatic periacetabular tumors. Distal femur resection with endoprosthetic reconstruction: a long run followup research. Modular uncemented prosthetic reconstruction after resection of tumours of the distal femur. Modular endoprosthetic reconstruction for decrease extremity skeletal defects: oncologic and reconstructive indications. Prosthetic knee replacement after resection of a malignant tumor of the distal part of the femur. Long-term outcomes of endoprosthetic reconstruction after segmental bone resection for bone tumors: analysis of 242 patients over 22 years of institutional expertise. Even in sufferers with metastases at prognosis, the 5-year survival rate has reached 20% to 30% due to chemotherapy and surgical procedure for metastases as properly as the first tumor. Limb salvage surgery for bone tumors within the immature skeleton creates unique issues. Maintenance of limb length after resection of one or more major development plates High functional and recreational demands of younger patients, which require a durable reconstruction At the knee, a constrained endoprosthesis is required (most commonly a fixed or rotating hinge implant), making it needed for the prosthesis stem to breach the physeal plate on the aspect of the joint opposite to the tumor. Reconstruction with expandable endoprostheses permits the maintenance of limb size equality, allows early weightbearing, leads to predictable function, has a low danger of early issues, and is readily available. Disadvantages include the expense of the prostheses and the problems which would possibly be expected to improve with time in surviving patients. The operated higher limb initially is longer, however the opposite limb quickly catches up. Patients whose estimated leg-length discrepancy is lower than three cm can be handled with typical "adult-type" prostheses made longer by up to 1. Recently, the validated multiplier technique has been proven to be a simple and accurate predictor of discrepancy. It could be computed using chronologic, not bone, age, and requires solely a single measurement. Terminal branches of the diaphyseal nutrient artery form tight loops close to the physis, and the epiphysis is invaded by juxta-articular vessels. During childhood, the physis turns into an avascular structure that lies between two vascular beds, one epiphyseal and the opposite metaphyseal. The epiphyseal vessels provide oxygen and vitamins; an intact epiphyseal vasculature is crucial, due to this fact, to sustain the chondrocytes. The metaphyseal vessels interact with the physeal chondrocytes within the hypertrophic zone and have to be intact to maintain normal ossification. Surgical methods for excision of the sarcoma are similar to these for adult tumors, which are discussed in later chapters (see Chaps. This chapter offers primarily with factors that must be thought of with the usage of expandable prostheses. We currently use two main methods of lengthening expandable endoprostheses in our heart. Their benefits and drawbacks are outlined in the following paragraphs (Table 1): the minimally invasive expandable prosthesis has been in use since 1993. The mechanism is encased within the prosthesis shaft, and the telescopic implant is extended utilizing an Allen key. A sealed motor unit inside the prosthesis contains a powerful magnet that can be activated by an external energy source (eg, a rotating electromagnetic field). This causes the magnet to turn, and the motor works utilizing a very-low-ratio gearing system (13061:1) to lengthen the prosthesis. The price of lengthening is immediately proportional to the length of time that the ability supply is utilized: lengthening of four. The physis on the opposite aspect of the joint may be both preserved using a "sliding" prosthesis or sacrificed and changed with a exhausting and fast cemented prosthesis. The sliding element is an uncemented, easy component placed via a canal made centrally in the remaining preserved physis. Care should be taken to decrease injury to the proximal progress plate by avoiding extreme periosteal stripping and thoroughly drilling out a cylindrical hole within the bone and, preferably, the middle of the physis. The proximal tibial physis is preserved, and the uncemented clean prosthesis slides inside the polyethylene sleeve because the physis grows. Illustration of the amount of growth of the proximal tibial physis 6 years after a distal femoral substitute with a sliding tibial component. The quantity of development can be seen by the expansion arrest line formed at the time of chemotherapy. The use of hydroxyapatite-coated collars has been shown to reduce the speed of aseptic loosening by encouraging bone ongrowth. A device developed by Kotz allows the prosthesis to be lengthened by a ratchet system that makes use of knee movement to trigger it to lengthen. When an influence source is utilized to the prosthesis, the wax melts and the spring extends. When the power source is eliminated, the wax solidifies and the spring is fastened in its new place. When an expandable replacement is being used, plan to exchange the precise amount of bone that has been eliminated. Ensure sufficient neutrophil and platelet counts previous to surgery if patient has had current chemotherapy (our unit requires a neutrophil rely larger than 1000/mm3 and platelet count of seventy five,000/mm3 or higher).

Buy cheap suhagra 50 mg line
The third incision is made anteriorly erectile dysfunction pills for diabetes cheap 100mg suhagra otc, and the tendon is delivered through a window in the interosseous membrane (just above the anterior inferior syndesmotic ligament) erectile dysfunction treatment home veda buy 50 mg suhagra overnight delivery. The fourth incision is remodeled the distal insertion of the peroneus brevis tendon erectile dysfunction protocol by jason buy 100 mg suhagra with amex, and the tibialis posterior is passed via a subcutaneous tunnel and woven into the distal peroneus brevis with nonabsorbable suture. A long-leg forged is used for 3 weeks and then a short-leg cast (weight bearing as tolerated) for a further 3 weeks. The patient may need extra procedures similar to osteotomy to restore alignment and movement. Weight bearing is typically delayed for 6 weeks, and an ankle�foot orthosis is worn after the solid is eliminated. An ankle�foot orthosis is usually recommended for up to 6 months after removing of the solid and may be required over the lengthy run to facilitate clearance if lively dorsiflexion is inadequate. Poor outcomes had been most typical in diplegics and quadriplegics, patients lower than 8 years of age, and these who had not achieved a group level of ambulation. A host of variables, including persistent spasticity, could end in progressive deformity by way of progress and growth, particularly in children with more profound levels of neuromuscular involvement. The approach involving break up tibialis posterior switch by way of the interosseous membrane has been the topic of two stories, in which 44 patients were studied at short- to mid-term follow-up. The switch helped to restore active dorsiflexion in a lot of the sufferers, eliminating the need for orthotics. Recurrent deformity outcomes from persistent muscle imbalance, pull-out of the tibialis posterior from the peroneus brevis, insufficient rigidity when suturing the tibialis posterior tendon, or other variables associated with development. Overcorrection into valgus is most typical in younger children and in patients treated by concurrent tibial derotational osteotomy. Long-term followup of surgery for equinovarus foot deformity in youngsters with cerebral palsy. Split posterior tibial tendon transfers in youngsters with spastic cerebral paralysis and equinovarus deformity. Tibialis posterior tendon transfer with concomitant distal tibial derotational osteotomy in youngsters with cerebral palsy. Effect of attachment site and routing variations in cut up tendon transfer of the tibialis posterior. Split posterior tibial tendon switch by way of the interosseous membrane in spastic equinovarus deformity. Split tibialis posterior tendon transfer in the treatment of spastic equinovarus foot. Preoperative and postoperative dynamic electromyography as an aid in planning tendon transfers in children with cerebral palsy. Changes in muscle second arms following split tendon switch of tibialis anterior and tibialis posterior. Effects of tensioning errors in split transfers of tibialis anterior and posterior tendons. Split tibialis posterior tendon transfer and tendo-achilles lengthening for spastic equinovarus toes. Other findings embrace contracted lateral and lax medial gentle tissues of the first metatarsophalangeal joint, lateral subluxation of the sesamoids, pronation of the good toe, and plantar subluxation of the abductor hallucis muscle. Complaints of ache over the medial exostosis or concerning the first metatarsophalangeal joint. The medial eminence is much less outstanding in adolescent bunions than in adult bunions. In older adolescents, where the physis of the primary metatarsal is closed, the corrective osteotomy could be performed proximally. If the physis of the first metatarsal is open, a primary metatarsal neck osteotomy has been described (Mitchell procedure). Goals are to lower ache and to restore the alignment of the primary ray, with respect to both the second ray and the joints of the ray itself. If feasible, surgery is delayed until early adolescence, as recurrence charges are higher in youthful youngsters. Approach A dorsomedial incision is made beginning just distal to the first metatarsophalangeal joint and increasing proximally for 5 to 6 cm. The stem of the Y is over the metatarsal, while the upper portion of the Y is formed distally. Leave the lateral portion of the joint intact to keep away from disrupting the blood supply to the top of the primary metatarsal. The first reduce includes removing the distinguished medial eminence with an osteotome, starting distally at the sagittal groove (groove of Clark). The second minimize is made on the distal metaphyseal�diaphyseal junction of the primary metatarsal. The third, proximal cut is made about 2 to three mm proximal to the first cut, and is created completely across the first metatarsal. The prominence of the distal portion of the metatarsal shaft is smoothed off with a rongeur, and a capsulorrhaphy is carried out with absorbable sutures. Sterile dressings are applied and the toe is splinted in impartial to slight plantarflexion. The first reduce of the osteotomy is carried out two thirds of the means in which by way of the first metatarsal on the junction of the metaphysis and diaphysis and is oriented perpendicular to the lengthy axis of the first metatarsal (line 2). The second bone minimize (line 3) is made fully through the bone and completes the osteotomy. It ought to be made 2 to four mm proximal to the primary cut and is perpendicular to the long axis of the second metatarsal. When seen from the medial aspect, the osteotomy should be oriented in order that a small plantar-based wedge is produced. This helps keep away from dorsiflexion of the distal fragment when the osteotomy is reduced. The surgeon ought to avoid resecting more than about 3 mm of bone to forestall shortening of the primary metatarsal. It should create a slight plantar-based wedge with the distal reduce to avoid dorsiflexion of the osteotomy. The modified Mitchell osteotomy (described above) produces 81% satisfactory outcomes, with no cases of malunion, nonunion, avascular necrosis of the first metatarsal head, infection, or transfer metatarsalgia. In older youngsters and adolescents there will be painful dorsal callosities about 50% of the time. There may also be issue find footwear that match appropriately in older kids and adolescents. Positioning the patient is supine, preferably with a bolster beneath the ipsilateral hemipelvis to make the lateral foot more accessible. The plantar handle should be slightly longer than the dorsal handle and directed slightly laterally. The extensor tendon is split, and a dorsomedial launch of the fifth metatarsophalangeal joint is performed. There ought to be no rigidity on the toe, and the toe should rest within the plantar deal with of the racquet incision.
Discount 50 mg suhagra mastercard
Instability at greater than 70 levels of flexion indicates injury to the collateral ligaments causes of erectile dysfunction in late 30s generic suhagra 100mg overnight delivery. Instability in extension indicates disruption of each the collateral ligaments and the volar plate erectile dysfunction 40s buy generic suhagra 50mg. The diploma of joint laxity suggests the extent of harm to the ligaments erectile dysfunction net doctor cheap 50mg suhagra free shipping, from microscopic tearing to full rupture. If the volar lip of the center phalanx has been fractured, minor tenderness over the dorsum of the center phalanx and greater tenderness volarly and laterally shall be present. Subtle fracture-dislocations could also be missed because of poor depiction of the areas of suspected pathology. The joint can be immobilized for a brief time to afford the patient comfort and to allow delicate tissue recovery. A dorsal splint is utilized to the digit at 20 to 30 degrees of flexion, avoiding immobilization beyond 30 levels to lessen the chance of flexion contracture. The length of immobilization reflects the minimal amount of time wanted to impact healing and procure joint stability. Extension block splinting allows early movement of a joint whereas preventing extension past an angle where instability is possible. A length of aluminum splint is then bent to an angle 10 or 15 levels larger than this level of redisplacement and secured to the dorsum of the hand with adhesive tape or as part of a short-arm solid. If the angle of the splint is larger than 60 levels, the arc of motion may be insufficient for the patient to achieve sufficient flexibility, and it might be essential to think about one other treatment routine. Successful results have been noted, nevertheless, with fractures involving up to 75% of the joint. As the fracture-dislocation heals, the extension block splint is progressively adjusted toward full extension, normally throughout a interval of three to 8 weeks. In sure situations, the digit may be too quick, stocky, or swollen for such treatment, or patient compliance and sophistication for such a regimen may be in query. Because of the potential for recurrent subluxation, the usage of conservative remedy should be matched with frequent and cautious evaluation of the joint. Serial radiographs should be obtained weekly to doc continued discount of the joint and progressive therapeutic of any fractures. Extension block splinting could additionally be just as effective in these milder instances, however, and it enjoys a decrease risk of joint contracture. The finger is simply too brief or swollen to fit appropriately into an extension block splint. He or she should pay attention to the chance that immobilization, splinting, and long-term rehabilitation may be needed. The affected person ought to be instructed to hold the injured hand clear before the process and to avoid extra pores and skin injury to decrease the potential for infection. Fingernails should be trimmed and cleaned and the hands totally scrubbed with antiseptic soap earlier than the operation. The surgeon ought to be comfy in the efficiency of a variety of alternative procedures and should have the necessary tools available should findings require an alteration in the authentic surgical plan. Dynamic skeletal traction methods, which use the precept of ligamentotaxis to maintain concentric joint reduction, are especially useful when the fracture is significantly comminuted. Drawbacks embrace the following: Significant prowess on the part of the surgeon is required, as are close postoperative supervision and adjustment. Volar plate arthroplasty, or the use of the distal aspect of the fibrocartilaginous volar plate to resurface the comminuted Positioning the strategy of getting ready, draping, and positioning the higher extremity is identical as for many hand surgical procedures. Approach Because extension block pinning is a percutaneous method, no approach is required. The wire is inserted in a retrograde direction, approximately 30 degrees off the long axis of the proximal phalanx. Alternatively, the K-wire can be placed to one side of the central tendon to keep away from tethering the extensor mechanism. Fluoroscopy is used to confirm a congruous joint discount following the procedure. If the joint continues to subluxate dorsally at extension, a V-shaped hole between the articular surfaces of the top of the proximal phalanx and the dorsal lip of the center phalanx might be seen on radiograph. The K-wire is left protruding by way of the bone, and its placement is confirmed by fluoroscopy. The insertion point for the K-wire can be located by a freehand approach after which confirmed with fluoroscopy. Easy passive flexion of the joint by way of an arc of 60 levels or higher ought to be confirmed following pin insertion. Gentle active range-of-motion exercises are allowed instantly and should be inspired generally. If the harm is especially serious-eg, injuries that required volar plate arthroplasty or that contained important comminution-immobilization for as much as 2 weeks may be indicated. The pin is eliminated 3 weeks after surgical procedure, and vigorous energetic flexion and extension are encouraged. Unstable fracture dislocations of the proximal interphalangeal joint: therapy with the pressure couple splint. Treatment of dorsal fracture/ dislocations of the proximal interphalangeal joint by volar plate arthroplasty. The long-term consequence of volar plate arthroplasty of the proximal interphalangeal joint. Acute open discount and rigid internal fixation of proximal interphalangeal joint fracture dislocation. Dorsal fracture subluxation of the proximal interphalangeal joints treated by extension block splintage. Extension splinting of palmar plate avulsion accidents of the proximal interphalangeal joint. Treatment of fracture-dislocation of the proximal interphalangeal joint utilizing extension-block Kirschner wire. The biological effect of steady passive motion on the therapeutic of full-thickness defects in articular cartilage: an experimental investigation within the rabbit. Extension block pinning for proximal interphalangeal joint fracture dislocations: Preliminary report of a brand new approach. The authors attributed the four circumstances with much less passable outcomes to using a 60-degree extension block splint postoperatively in a single patient and important comminution in the different three patients. One case involved a 45% single fragment fracture seen 1 day postinjury and another a 35% comminuted fracture seen 17 days post-injury. Following pin removal and 1 month of passive and lively workout routines, each patients regained full vary of movement. Convex-side injuries are usually simple (two-fragment) injuries greatest treated with open discount and inside fixation if surgery is required.
References
- Grasso AW Barman N. Cardiac tumors. In: Griffin BP, Topol EJ, eds. Manual of Cardiovascular Medicine. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2009:288-293.
- Bruera E, Pereira J, Watanabe S, et al. Opioid rotation in patients with cancer pain. A retrospective comparison of dose ratios between methadone, hydromorphone, and morphine. Cancer 1996;78(4):852-857.
- Van der Zwan A, Hillen B, Tulleken CAF, et al. Variability of the territories of the major cerebral arteries. J Neurosurg 1992; 77:927.
- DiMichele DM, Lasak ME, Miller CH: A study of in vitro factor VIII recovery during the delivery of four ultra-pure factor VIII concentrate by continuous infusion, Am J Hematol 51:99, 1996.
- Kimura M, Amino N, Tamaki H. Gestational thyrotoxicosis and hyperemesis gravidarum: possible role of HCG with higher stimulating activity. Clin Endocrinol 1993; 38: 345-50.
- Piela N, Kornweiss S, Sacchetti A, et al: Outcomes of emergency department placement of transvenous pacemakers. Am J Emerg Med 34(8): 1411-1444, 2016.
- Zhou XY, Willemsen R, Gillemans N, et al. Common point mutations in four patients with the late infantile form of galactosialidosis. Am J Hum Genet 1993;53:966A. 80.
- IOM Committee Report on Sodium Intake in Populations. [(Accessed on 25 August 2013)]. Available at: http: //www .iom. edu/R eport s/201 3/Sod ium-I ntake -in-P opula tions -Asse ssmen t-of- Evide nce.a spx. Accessed on 24 April 2017.

